In my Clinical Nurse Specialist role within an acute care setting, I work each shift in close partnership with graduate nurses. This team-based model pairs us together in meeting patient care requirements and graduate learning objectives.
Most of these shifts also involve me supporting an undergraduate student simultaneously; I act as a formal preceptor to both.
These tasks of mentorship, assessment, and clinical oversight have provided me with valuable perspectives that continuously remind me of the complexities of supporting emerging clinicians.
One common yet often misunderstood aspect of providing this support is performance management.
This phrase is often accompanied by tension as some view this as evoking corrective actions. Others may perceive that it is, in fact, a structured way of monitoring progression.
In the context of graduate nurses, performance management has the unique role of ensuring safe, quality care whilst nurturing skill development, confidence, competence and professional identity. Balancing these elements is not often easy.
My experience shows that focusing less on what graduates are 'doing wrong' and more on how we, as clinical leaders, can shape our expectations helps better align with this development stage.
Graduates: Forming their clinical identities
Completing a university degree does not make a graduate nurse fully formed and autonomous; in fact, they are emerging clinicians.
In complex and rapidly evolving healthcare settings, graduates are still learning how to connect theory to practice, refine time management, and interpret complex clinical cues.
Navigating a new profession, performing these new tasks, and refining a professional identity is naturally accompanied by nerves, excitement, and, of course, some bumps along the way.
Applying traditional frameworks with rigid approaches risks the assumption of confidence or resilience, which is still developing in these graduates. While we may view traditional performance conversations as constructive, graduates may very well perceive them as criticism if feedback is not well aligned with the developmental context.
This is where mentoring up is relevant. Providing a structured framework that highlights the reciprocal and evolving nature of mentorship promotes innovative, tailored support.
Considering each graduate's individual journey through professional formation rather than imprinting our expectations upon them can remind us that mentorship is not a delivery requirement but a co-creation between mentors and mentees across their developmental stages.
Accountability feels different as you grow
My experiences have shown me that graduate nurses don't avoid accountability.
In fact, most of them are deeply invested in achieving goals, meeting expectations, and becoming safe, competent clinicians. This makes our methods for framing accountability even more important.
Emerging clinicians are juggling learning task prioritisation, effective delegation, and complex clinical management. Pair this with performance discussions that are not underpinned by support, and it's no surprise that feelings of overwhelm and anxiety can emerge. Graduates may perceive that these conversations are taking place because they are not coping, when the reality is that we know they are still learning.
Self-reflection is powerful here. When we, as clinical leaders, create a space for self-reflection, graduates are empowered to examine their choices, understand context, and actually link their pre-established theory into clinical reality. This promotes the conversion of lived experiences into practical comprehension, which is pivotal in clinical judgment and professional identity formation.
Capability in contribution: let's support, not scrutinise
Recently, I was reading through some contemporary evidence on graduate nurse capability, which reminded me of the well-known concept of workforce capability. Whilst defined in many ways, it relates to the collective knowledge, skills, abilities and attributes of nursing which are required for safe, effective, quality patient-centred care delivery.
Through the frame of workforce capability as a whole, we see how graduates, although limited in their experience, hold individual competence that actively contributes to their team's capacity.
Their contribution to collective workforce strength should be acknowledged and supported; we cannot measure graduates against the same rubric as experienced nurses. Their performance is within a different yet still important development stage that requires a complementary, although not identical, assessment approach.
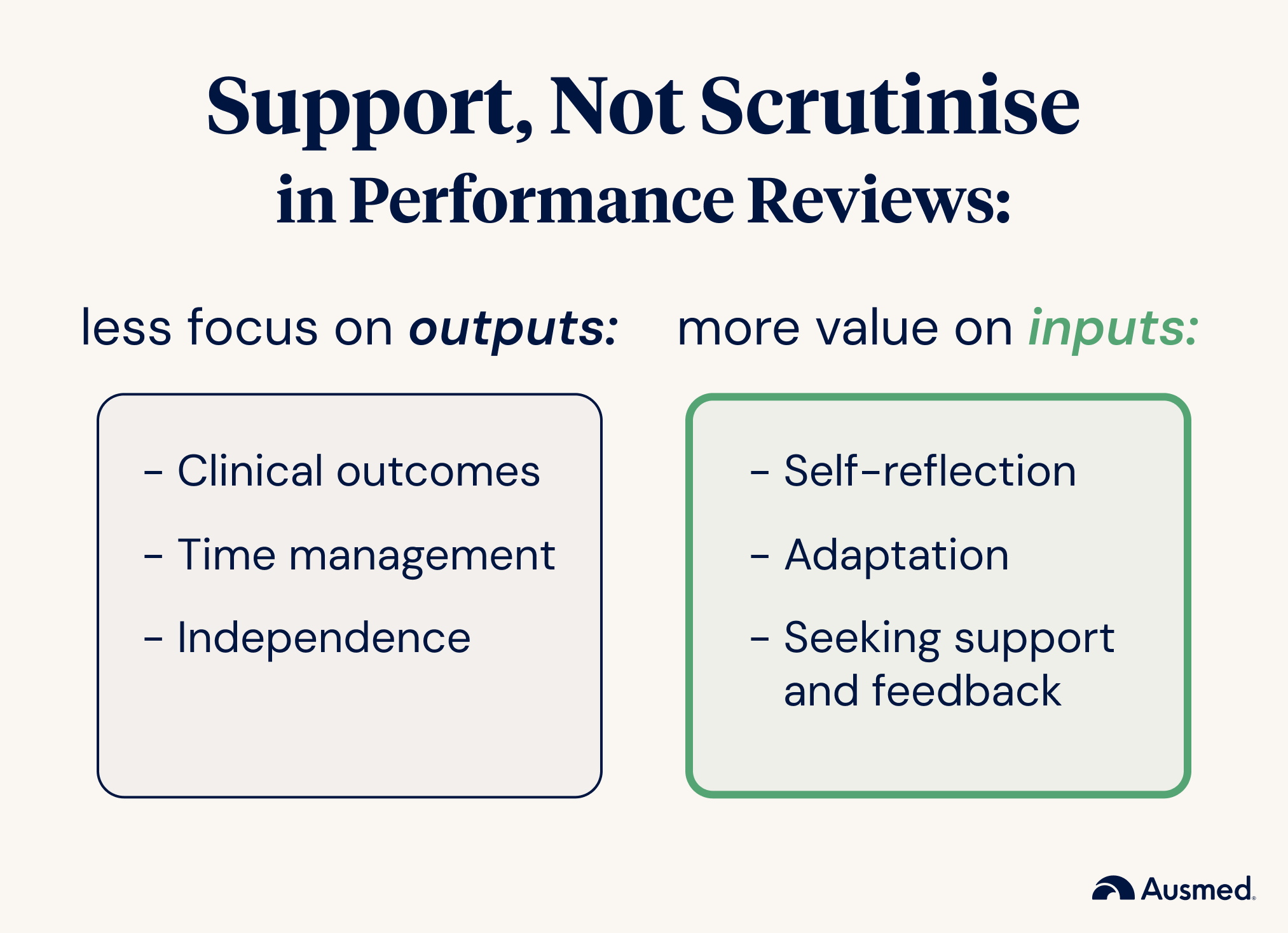
In this context, I find it useful to shift from focusing on outputs revolving around clinical outcomes, time management, and independence to valuing inputs like self-reflection, adaptation, and seeking support and feedback. I'm sure I'm not the only one who views these as strong indicators of a graduate's long-term potential rather than judging them based on their ability to complete tasks with perfection while under pressure.
Personally, I see how shifting mentor perspectives can transform a graduate's experience as they flourish. I choose to celebrate their growth rather than highlighting deficits. This embraces and encourages their accountability, self-awareness, and engagement in their own development, as they know they are supported, not scrutinised.
With this approach, we are not lowering standards on the provision of safe care; we are simply calibrating support and assessments to match contextual developmental needs. This nurtures progression rather than penalising inexperience.
Let's reframe performance management
My experience is that graduate nurse performance management is optimised when it's relational rather than transactional.
This is because great benefits are reaped when feedback feels like an open dialogue stemming from trust, curiosity, and mutual respect.
This begins with appreciating each individual graduate for their unique learning style, background, and concerns. This process involves inquiry before judgement and encourages self-reflection before feedback.
By way of an example, instead of leading with 'This requires improvement', I like to begin with 'Can you explain to me how you approached this?'.
Opening exploratory dialogue centred on clinical judgement and critical thinking enables these moments to form professional identity and insights. This method of performance management reinforces how learning is expected, growth takes time, and that challenge doesn't define competence; it builds upon it.
This then nicely aligns with mentor up in emphasising mutual engagement for mentors and mentees to navigate these clinical setting complexities.
Supporting growth while ensuring safe care
Upholding quality patient care is imperative, but so is supporting the emotional safety of graduate nurses.
The good thing is that I have found that graduates who feel safe and guided are more open to accepting feedback and more reflective and accountable when they do not feel judged.
Additionally, recent studies have demonstrated that graduate programs designed to improve the critical reflection of experienced nurses across all career stages increase their own critical thinking and teaching abilities.
Embedding critical reflection into performance management dialogue encourages graduates to explore actions and decisions as developmental milestones. This encourages inquiry like 'what happened' and 'why did it happen like this,' which builds on their critical thinking and confidence by asking 'what could I change next time?'
Equipping mentors to act with strong, enlightened capabilities underscores the importance of highlighting practical strategies that they can then use to guide graduate reflection throughout busy shifts in theory and practice.
Shifting our role from evaluator to enabler
My clinical, teaching, and PhD experiences have shown me that performance management across graduate programs is not a process but a relationship built on trust and shared goals.
This approach recognises that learning and transformation are essential throughout a nurse's professional journey; my support heavily influences graduates' clinical development and perceived self-image.
Shifting our engagement with graduates and reframing ourselves as mentors enables us to embed reflection and guidance into all of our graduate nurse interactions. Careful construction of our performance management views and processes creates a ripple effect of graduate development, which leads to their increased role satisfaction and patient care quality.
This strategic shift can not only improve individual experiences but also the future of nursing.
Final reflections
Walking alongside graduates with empathy and advice supports them through these formative nursing career stages.
I recognise that performance must be managed and standards upheld. However, leading with empathy and clarity transforms performance management from being potentially deflating into a meaningful developmental experience.
Mentoring up reminds us of this, and how mentorship is reciprocal and contextual as a roadmap for mutual growth and a professional responsibility for all nurses through career progression.
Remember that critical reflection highlights growth and assigns meaning through experiences, which transform theory into practice.
When experienced mentors feel empowered to facilitate this reflective practice with intent, but not leniency, performance conversations can naturally shift from critique to guidance.
As mentors, we require the innate understanding that although graduates are registered nurses, they are also at the beginning of their careers, and the feedback we provide is about continuous dialogue rather than single events.
Delivering performance management with care, clarity, and curiosity moves this process from measuring progress to facilitating growth, which is one of the most meaningful forms of support we can provide.



