The Royal Commission into Aged Care Quality and Safety showed serious cracks in the governance of some aged care organisations, particularly regarding accountability, transparency, and board oversight of quality and risk.
In response, the Aged Care Act 2024 introduces sweeping governance reforms that clearly define the legal responsibilities of board members, executives, and other “responsible persons.”
This article explores:
- The key governance changes under the new Act
- What boards are now responsible for
- How transparency is being built into decision-making
- The board’s growing role in driving continuous improvement
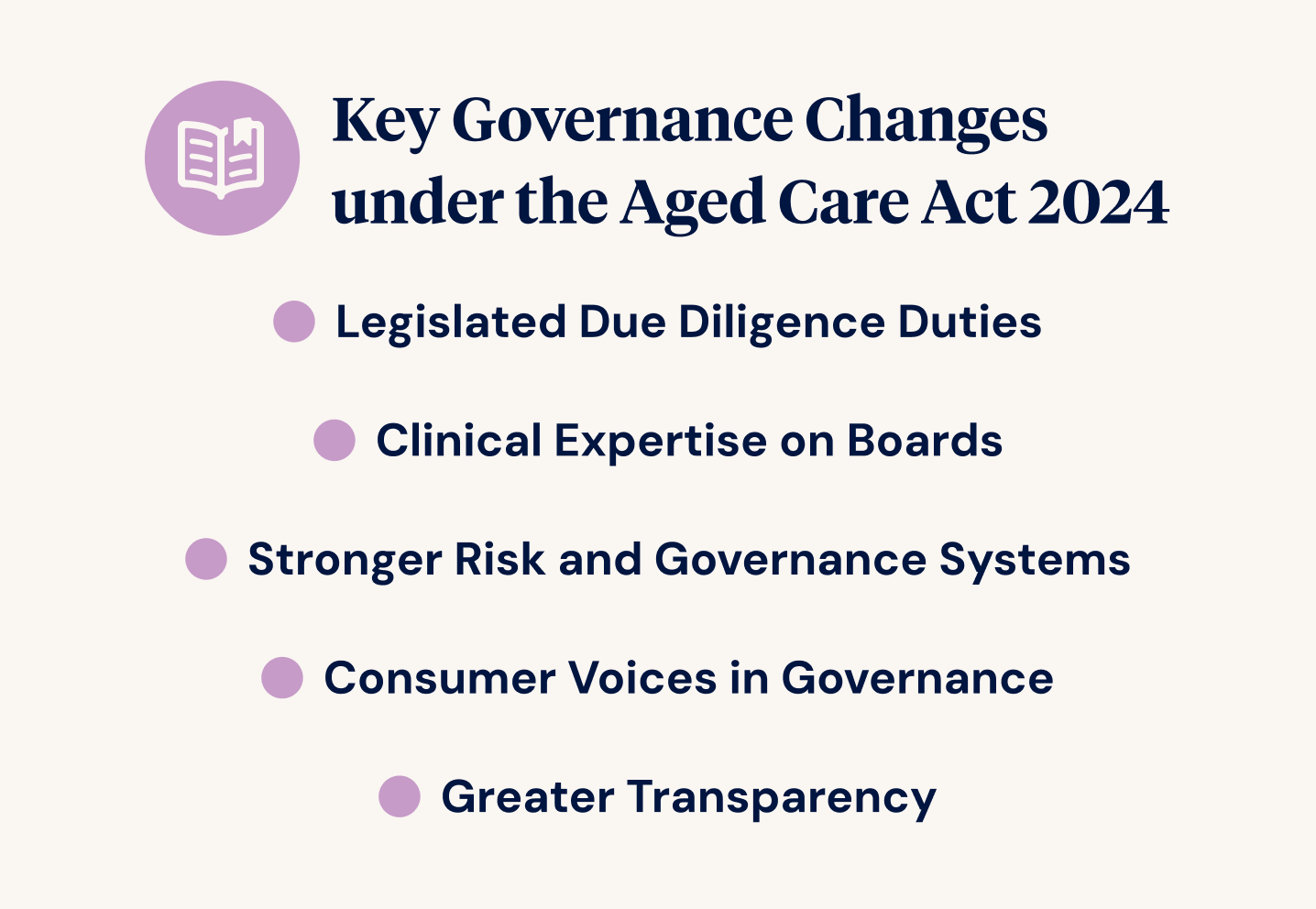
Key Governance Changes Under the Aged Care Act 2024
The new Act lifts aged care governance to a higher standard, drawing it closer to the expectations already seen in healthcare and financial services. It moves from vague notions of accountability to complex legal duties for those in charge.
Notable changes include:
Legislated Due Diligence Duties
Directors and executives are now expected to actively ensure compliance and take reasonable steps to meet the new Provider Duty. Ignorance or inaction is no longer an excuse.
Clinical Expertise on Boards
Every governing body must now include at least one member with clinical or care experience, which helps boards make more informed decisions that centre on individuals’ wellbeing.
Stronger Risk and Governance Systems
Providers must maintain robust risk and quality systems, with clear processes for escalating and responding to incidents.
Consumer Voices in Governance
Individuals and families must be meaningfully involved in governance, reflecting a stronger focus on rights and person-centred care.
Greater Transparency
Providers must publish information about their governance, service quality, and finances, including new public reporting obligations.
Board Responsibilities and Accountability
Board members are responsible for safety, quality, compliance, and culture. Their role has expanded far beyond traditional oversight.
Boards are now expected to:
- Keep governance frameworks current, documented, and reviewed annually
- Respond to reports about incidents, complaints, and risks
- Oversee executive performance, especially how it links to care quality and compliance
- Ensure codes of conduct, conflict-of-interest policies, and whistleblower protections are in place
- Regularly assess board skills and effectiveness, and take action to improve
Building Transparency Into Decision-Making
The Act prioritises visibility. Making the right decisions is not enough—boards must be able to show how and why those decisions were made.
Recommended practices include:
- Publishing governance frameworks on the provider’s website
- Clearly showing how strategic priorities link to consumer outcomes and risk management
- Sharing regular summary reports with individuals and families
- Making sure board minutes show who was consulted, what evidence was considered, and what feedback influenced the decision
Transparency fosters trust, not just with individuals, but also with staff, regulators, and the community.
Governance Tip
Use a simple “decision log” that records:
- The issue
- Who was consulted
- Risks and rights considered
- Evidence used
- Key discussion points
- Final decision and follow-up actions
Boards and Continuous Improvement
Good governance isn’t just about avoiding mistakes but pushing for better. The Act calls on boards to be active drivers of improvement across care, culture, and resident experience.
Practical steps include:
- Supporting and funding annual Quality Improvement Plans
- Creating a Quality and Risk Committee with clear responsibilities
- Tracking trends in incidents and complaints to spot broader problems
- Asking management to report on resident quality of life, not just clinical indicators
Strengthening Board Capability and Culture
Legal duties are essential, but strong governance also depends on the people at the table and how they work together.
Good boards:
- Participate in annual training, including on new legislation and risk frameworks
- Make space for diverse perspectives, including the lived experience of care
- Ask tough questions like, “Are we doing what’s right?” rather than just, “Are we compliant?”
- Commission external board evaluations every two years to uncover blind spots
The Risks of Weak Governance
Poor governance isn’t just risky, it can be costly and even unlawful.
Risks include:
- Civil or criminal penalties for directors
- Loss of accreditation and funding
- Damage to reputation and occupancy
- Staff disengagement and high turnover
Boards must lead proactively, not wait for their first audit or a crisis.
The New Governance Standard
The Aged Care Act 2024 message is clear: governance must be active, skilled, transparent, and accountable. Boards are no longer a step removed from care quality. They are a central part of it.
Good governance:
- Improves care outcomes
- Supports and retains staff
- Builds community trust
- Reduces risk and strengthens long-term sustainability
This is a new era of leadership in which boards must match good intentions with strong systems, reflective practice, and a genuine commitment to putting individuals first. That’s how we rebuild aged care, one decision at a time.
Want to learn more?
Explore Ausmed’s Governance resources and more reading on:



