Introduction
With the new Aged Care Act now scheduled for November 2025 and the Strengthened Quality Standards set to accompany it, aged care providers face not just compliance pressures but a genuine opportunity for strategic realignment.
The sector’s response to the delay has been mixed. While some providers expressed relief, others have voiced their frustrations.
Good governance in transition means asking: Are we not only ready to change, but ready to lead differently?
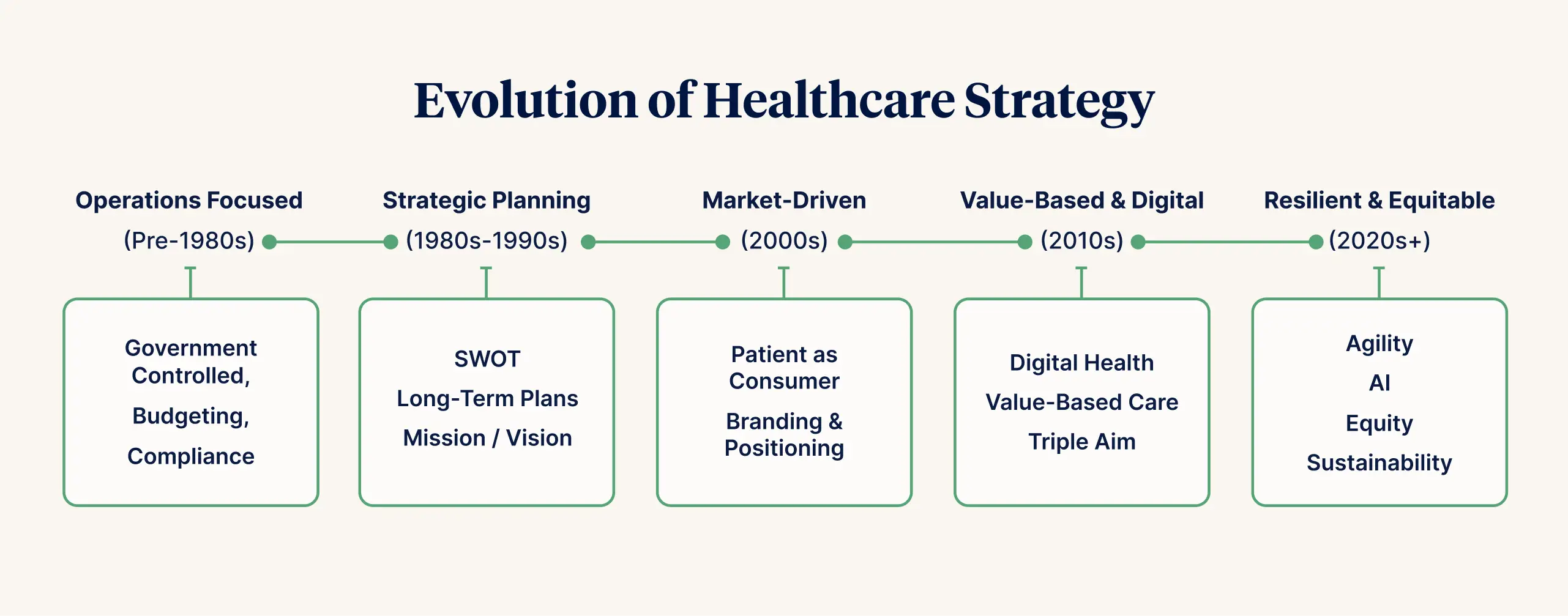
In this thought leadership piece, I invite you to embrace this pause as an opportunity to appreciate the significant evolution in how healthcare providers have approached strategy and how reforms such as sociopolitical, technology, consumer expectations, and global health challenges have shaped how we think about strategy today.
I invite you to take a moment to review what forces are shaping your strategy and how well it is serving your organisation's mission and purpose. Then, explore the opportunities to approach your strategy differently during this time of reform.
Defining Strategy
Strategy is one of those words that generates different thoughts, images and feelings for different people. My image for strategy is that at its heart, strategy is the bridge between purpose and impact (real-world outcomes).
✔️ It starts with clarity of intent. What outcomes we’re here to create.
✔️ It flows through choices. What we will and won’t do.
✔️ And it lives in capability. What our people need to know, do, and be to make that intent come alive.
I think of it like a value chain:
- Purpose → we want safe, person-centred, dignity-driven care
- Design → so we focus on enabling teams, leadership behaviours, and systems for learning
- Capability → we build skills, cultures, and technology that support this vision
- Impact → and we measure what truly matters: not just throughput, but real-world outcomes.
In transitioning to the new aged care reforms, the goal is an outcome-based strategy; it’s not just service delivery but value creation.
Reframing how we think about strategy, through the lens of a value chain, can help shift our mindset from planning to outcomes, connecting intent to impact.
The Tight–Loose–Tight approach to Healthcare Strategy
We all appreciate that healthcare doesn’t operate in a vacuum. It’s a system of tensions:
- Clinical vs. financial
- Individual rights vs. population health
- Innovation vs. risk management
Effective strategy in a high-performing or high-reliability context doesn’t erase those tensions; it works with them.
One powerful way to approach strategy in a complex system is what’s known as tight–loose–tight. It can be especially helpful in healthcare, where complexity and competing logics are the norm.
Here’s what it could look like:
Tight on Purpose
Be uncompromisingly clear on the why. Be unequivocally clear about outcomes, values and direction. This includes shared values, outcomes that matter to people, and what success looks like.
Loose on Method
Give teams flexibility and autonomy to experiment, adapt, and use their judgment on the ‘how’. Trust local teams to innovate, adapt and respond to context.
Tight on Accountability
Hold a shared commitment to measuring what matters. Set shared indicators, reflection cycles, and feedback loops that track impact, not just activity. Ensure that the learning flows both up and down.
It is important to note that tight-loose-tight is not micromanagement; it isn’t about controlling people. It is about mission clarity paired with operational trust; it’s about giving permission.
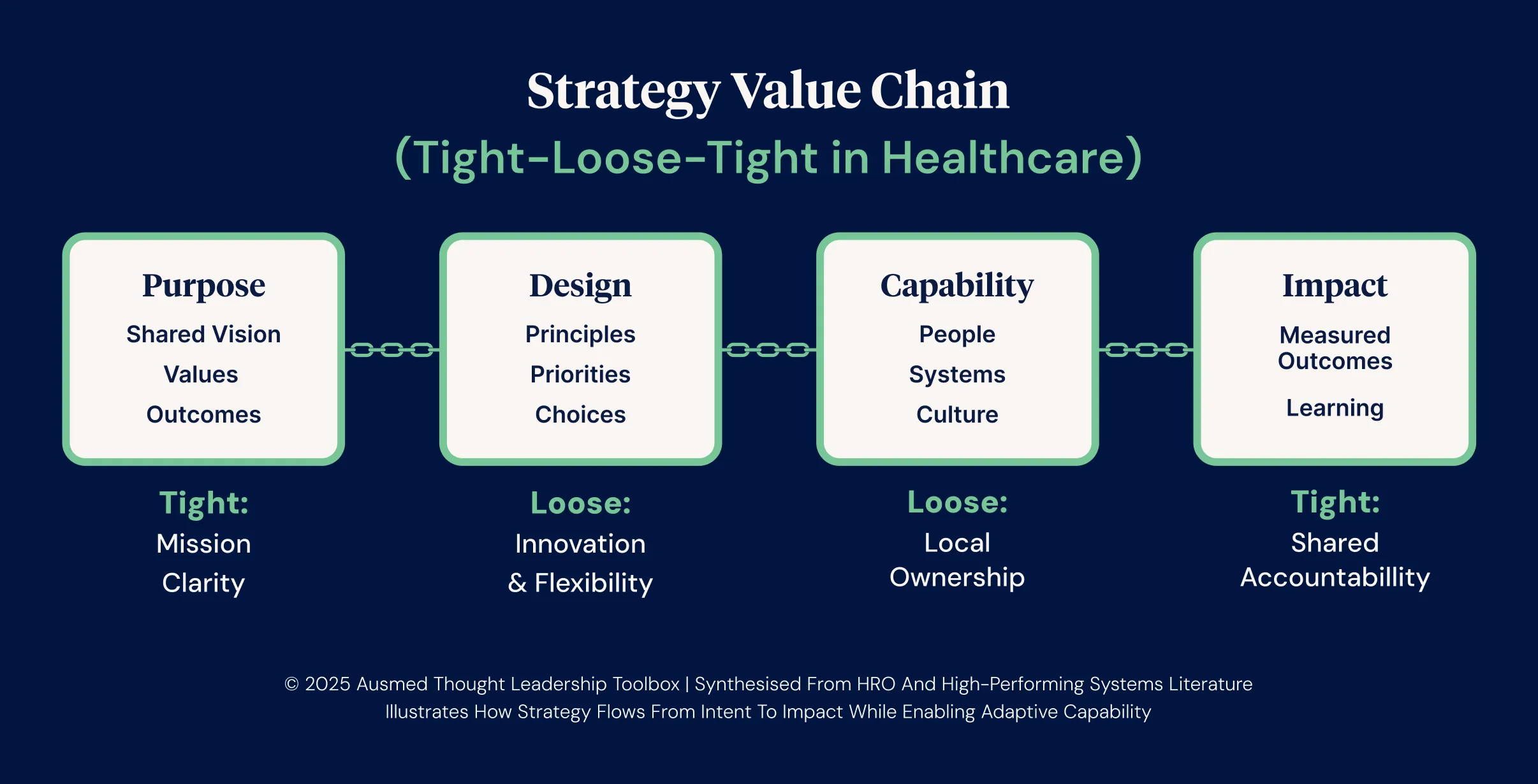
The Strategy Value Chain illustration reflects the mindset often associated with High-Reliability Organisations (HRO): decentralised decision-making, a commitment to continuous learning, and an ability to navigate complexity without becoming chaotic.
For this framing to work well, there needs to be space and safety for “strategy moments.” Rather than treating strategy as an executive function, strategy conversations are encouraged at all levels and embedded in everyday practices such as reflective practice, team huddles, morbidity and mortality meetings, and capability planning cycles.
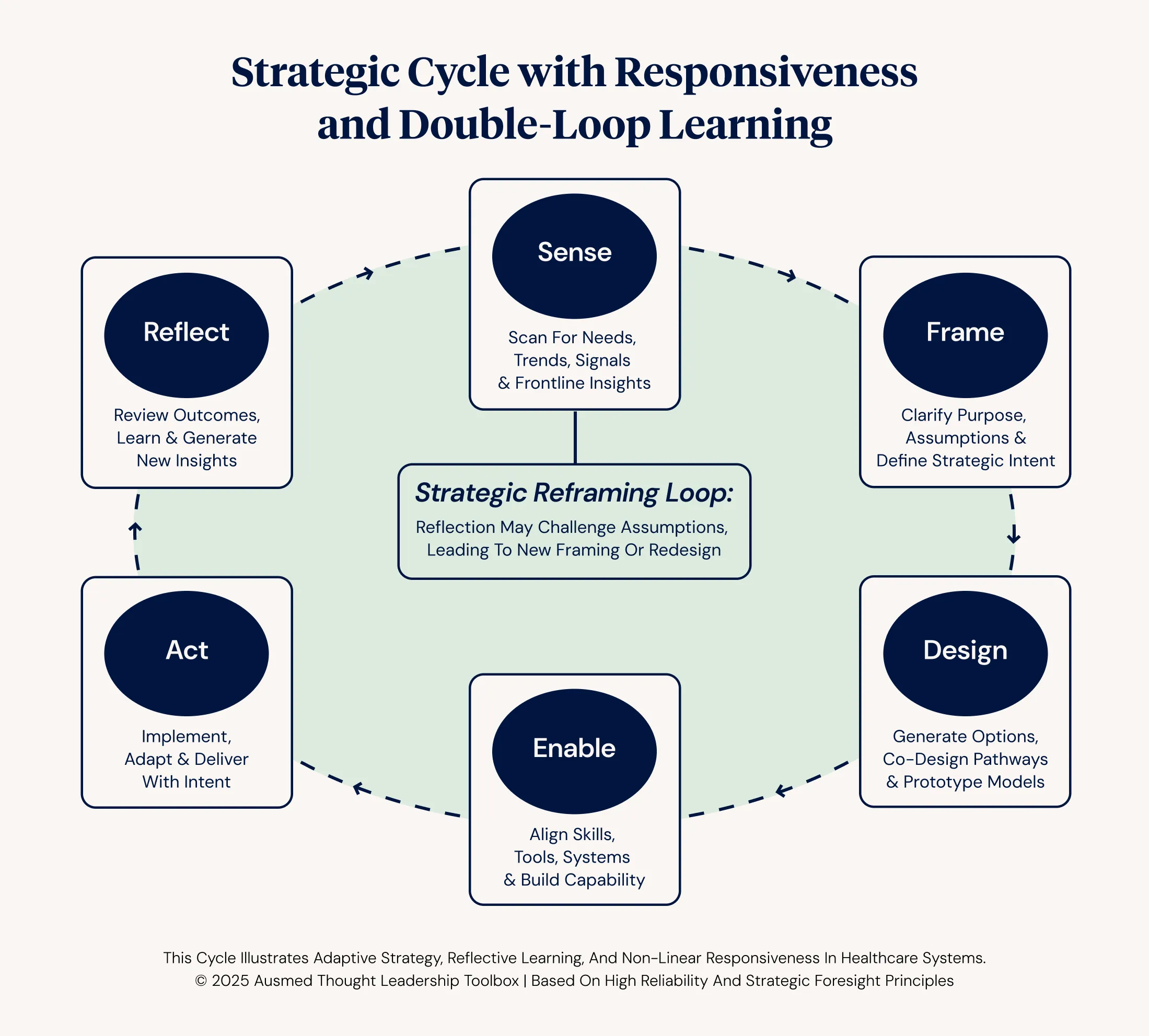
From Static Plans to Strategic Cycles: Foresight in Practice
In preparing for the multiple possible futures that health and legislation reform present, strategy becomes less like a script and more like a compass, designed to guide in shifting conditions.
The traditional 3, 5 or 10-year strategy model has been shown to struggle to keep pace with reform, disruption and demographic shifts. Instead, leading systems are adopting strategic foresight tools such as:
- Scenario planning: Developing multiple plausible futures and preparing for each.
- Signal scanning: Watching emerging trends and for weak (smoke) signals of change.
- Strategic rehearsals: Running 'what if' scenarios to test readiness and agility.
These tools invite us to shift from prediction to preparedness. They support a mindset of curiosity, humility and resilience, which are hallmarks of high reliability and high performance.
A Strategic Cycle for Healthcare Organisations
Karl Weick’s work on HROs emphasises sensemaking, the active process of framing, interpreting, and re-framing messy, conflicting inputs before acting. This is essential in environments such as healthcare, which hold competing logics (e.g. clinical care vs. business performance vs. compliance).
You can’t manage complexity with clarity unless you first acknowledge its ambiguity.
To support strategic maturity, organisations can consider adopting a simple, repeatable cycle:
- Sense - Observe systems, needs, data, and emerging trends.
- Frame - Clarify purpose, define challenges, and agree on outcomes.
- Design - Develop options, include voices, and shape pathways.
- Enable - Align capabilities, systems and supports.
- Act - Implement and test with intention.
- Reflect - Learn, adjust, and scale what works.
This cycle fosters a culture in which strategy is not a static or annual event but a continuous, reflective, and adaptive process that enables responsiveness and learning.
Strategic Planning for Reform
Strategic planning for reform is not the same as annual business planning. It requires organisations to navigate uncertainty, engage stakeholders early, and prepare for shifts that are cultural as much as operational.
It’s not just about “how to comply” but how to transition well, sustainably, inclusively, and with capability uplift embedded from the outset.
| Characteristic | Explanation | Practical Example |
|---|---|---|
| Foresight-based | Assumes the future is not linear. Uses scenarios, not timelines alone. | Use multiple planning assumptions: e.g., “If home care is rights-based…” |
| Co-designed | Engages consumers and staff in shaping future models of care. | Host planning labs or roundtables with residents, carers, and workers. |
| Standards-aligned | Maps organisational priorities to the new Quality Standards domains. | Embed Standard 6 (Feedback & Complaints) into early change design. |
| Transition-governed | Uses a dedicated governance stream or establishes a transition committee to oversee progress. | Monthly strategy transition progress group with a charter, updates to the Board and wider organisation |
| Capability-integrated | Links reforms to education, supervision, systems and measurement. | Develop learning plans as a direct output of strategy review. |
Transitional governance is a key feature of an effective reform strategy. Leading systems often implement:
- A transition committee or board sub-group with a charter including transparency.
- Milestone maps tied to strategic objectives and capability uplift
- Use of readiness indicators, not just project plans, to gauge progress
- A regular rhythm of reflection and adjustment (e.g. tight–loose–tight cycles)
This supports alignment between service redesign, compliance, workforce development, and strategic intent.
Embedding Strategy Through Capability
In my view, one of the most overlooked truths in healthcare strategy is this: capability is not a downstream issue. It’s the connective tissue between what we say we value, and what we actually make possible.
Building workforce capability is how strategy becomes culture, whether it's engaging clients and carers in care planning, supporting a nurse to lead improvement, or helping a team make sense of data.
If our people can't see themselves in the strategy, we don't have one.
Summary: Strategy guided by Trust in times of Complex Reforms
At its core, strategy is about clarity, adaptability, and foresight. It’s about aligning our vision with actionable plans, building capabilities across the health workforce, and embracing innovation to meet the evolving needs of our communities.
Effective reform requires a willingness to make change happen. This generally requires trust in the intentions and expertise of both the designers and the implementers of any given strategy. Trust is a dynamic, relational and human quality. It takes time to develop, but can be broken in an instant. By keeping our strategies human-centred and flexible, we can build trust whilst ensuring that our healthcare system remains resilient and responsive as we transition towards bringing the aged care reforms to life. The following principles are not exhaustive, but my bias is that they hit the spot and can serve as a guide.
| Principle | Explanation | Example in Practice |
|---|---|---|
| Human-centred | Strategy grounded in lived experience (patients & staff) and relationships | Involving carers in dementia strategy & service design |
| Learning-oriented | Reflection and responsiveness to feedback, failures & success. Using data insights and rapid adaptation | Weekly team huddles that review what’s working |
| Shared and distributed | Informed by many voices, enacted through many roles | Capability planning in local services |
| Foresight-driven | Oriented toward multiple futures, not fixed predictions | Scenario planning workshops with emerging tech, climate, AI inputs |
| Relationally accountable | Strategy guided by trust. Balancing metrics with meaning, and strategy with stewardship | Co-designed scorecards with consumers and staff |



