Why Storytelling Matters
Storytelling, supervision, and education are deeply connected. Storytelling is so powerful that it is its own kind of specific therapy - Narrative Therapy. This therapy involves a respectful, non-blaming approach to counselling and community work that centres people as experts in their own lives (Dulwich Centre, 2025). Similarly, Dialectical Behavioural Therapy teaches that people can look at situations differently and that all ideas are valid (Sane, 2025).
At their heart, these therapies:
- Provide a safe space to speak.
- Foster active listening and validation.
- Encourage reflective and strengths-based questions.
The Overlap Between Storytelling and Therapy
The principles of education and storytelling overlap, mainly through clinical supervision. Storytelling helps clinicians broaden their perspectives, process complex experiences, and deepen their capacity for empathy.
- Storytelling helps individuals reflect and find meaning.
- Supervision offers a safe, structured environment to share and explore these stories.
- Education becomes the vehicle through which reflective practice and growth are nurtured.
In this guide, I share insights from my clinical practice and lived experiences, illustrating how storytelling and education are intricately linked and how organisations can practically instil adequate clinical supervision into the workplace.
Storytelling in Education: The Power of Supervision
With this in mind, we should appreciate the value of storytelling as a formal mode of education. Storytelling helps clinicians hear and broaden their perspectives and abilities to empathise.
Most times in life, when something seems too good to be true, it is. But I promise you, effective clinical supervision is one of the exceptions to the rule!
Clarifying Supervision
Despite its name, clinical supervision is not about overseeing practice; it’s about nurturing reflection, support, and self-care (Australian Nursing and Midwifery Federation, 2025).
Clinical supervision (or mentorship, as I like to think of it) is a formal method of storytelling in healthcare. Done well, it:
- A supportive, strengths-based, positive and nurturing experience
- Enables health professionals to reflect on clinical experiences with an experienced and trusted supervisor.
- Facilitates slow thinking, which helps the clinician process emotional, ethical, and complex aspects of practice.
- Improves staff retention and staff satisfaction and reduces burnout (Australian Clinical Supervision Association, 2025).
Clinical supervision is not:
- Expensive: It can be in-house and doesn’t always need an external facilitator.
- Time-consuming: You don’t need to take much time out of the workday to do it.
There are no reasons why clinical supervision can’t be embedded into all health care settings. Any activity, like supervision, that reduces staff burnout will pay enormous dividends, both in the short and long term.
Why Emotional Processing Needs Support
Supervision is essential because to process something emotionally, we need a quiet space and often, support around us. Clinicians are not usually able to emotionally process anything that happens at work, because let’s be honest, it’s rarely a quiet day.
Without clinical supervision, many clinicians experience difficult things at work and are left to try to deal with them on their own after they get home. Often, the stressor is left mentally unresolved, and then the clinician carries this burden to work the next day. Then, more and more stressful events occur; consequently, stress accumulates.
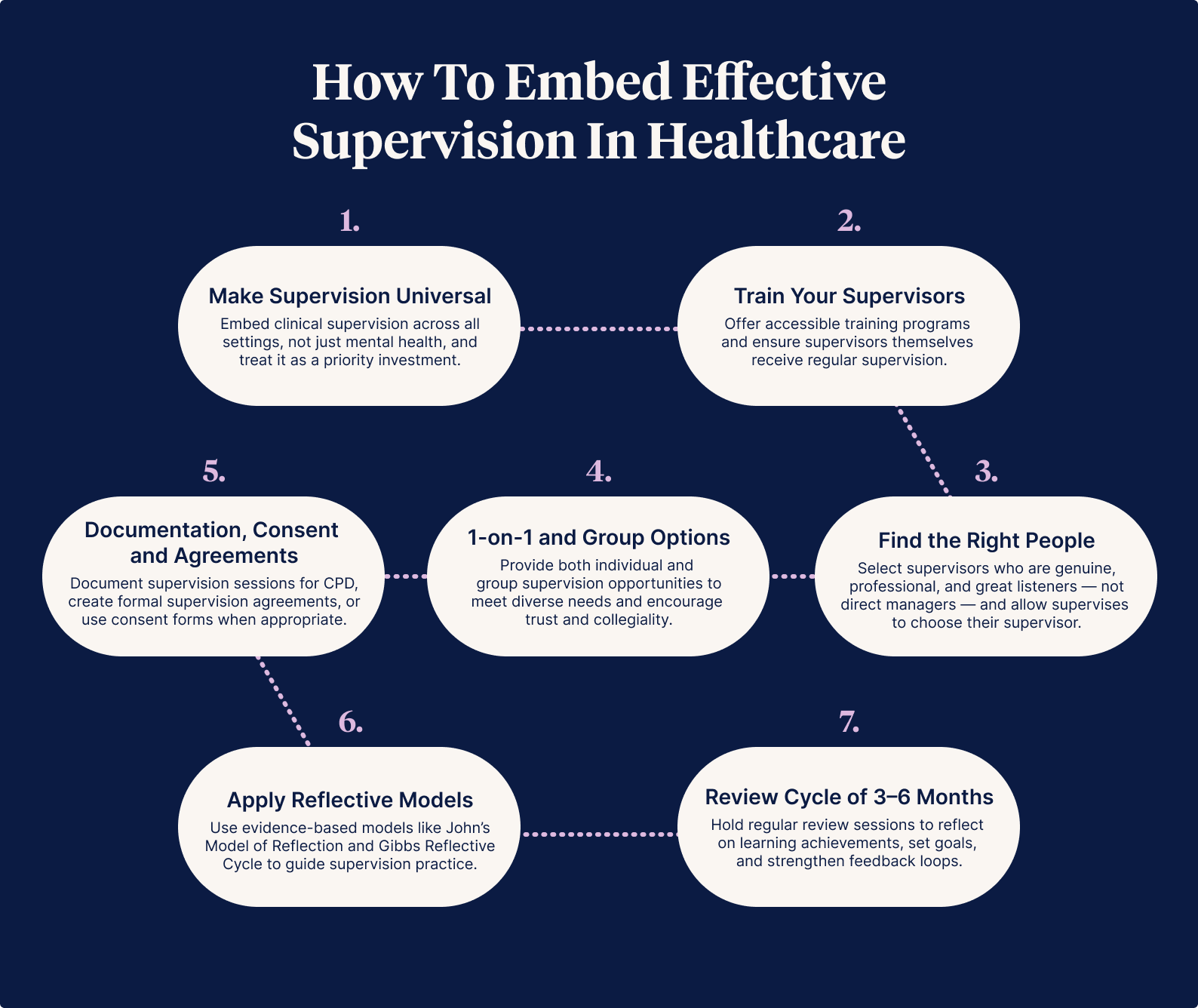
How to Embed Effective Supervision in Healthcare
I thought I might become a trauma sponge when I became a clinical supervisor. But like how it is when I do therapy with my clients, I've found it's an enriching experience.
Clinical supervision should be in all healthcare workplaces!
Drawing on my experiences as a clinical facilitator, mentor, and supervisee, here are practical ways healthcare workplaces can strengthen supervision practices
1. Make Supervision Universal
It was only when I started working in mental health that I discovered clinical supervision. In mental health nursing, clinical supervision is mandatory (monthly at a minimum).
- Embed clinical supervision across all settings, not just mental health.
- Treat time for supervision as a priority investment.
When individuals have a positive first experience in supervision, they are more likely to open up in future sessions.
2. Train Your Supervisors
There are plenty of clinical supervision courses available for your staff to attend.
- Offer 1–2 day training programs (e.g., Clinical Supervision Services; Bouverie Centre).
- Ensure supervisors themselves have supervision.
Each clinical supervisor also needs their own clinical supervision to work through their personal and professional hardships and reflect on their practice as clinicians and clinical supervisors.
3. Find the Right People
A clinical supervisor should be a good listener who can be genuine while staying professional and kind.
- Avoid supervisors being direct managers (conflict of interest).
- Allow supervisees to choose their supervisor.
Sharing your lived experience with your supervisee while ensuring you do not make the session about you can help your supervisee develop trust and rapport by humanising the experience.
Clinicians should be empowered to see a different supervisor if they don’t feel their existing supervisor is a fit.
4. One-on-One versus Group Supervision
To weigh up what might suit each individual:
- One-on-one: Builds safety and trust.
- Group: Encourages collegiality; requires an encouraging facilitator.
One-on-one supervision often helps clinicians feel safe speaking about things that make them feel vulnerable.
This form of clinical supervision also provides a beautiful opportunity for the supervisor and supervisee to get to know each other meaningfully.
On the other hand, group or peer supervision encourages staff collegiality in a supportive space, with a facilitator guiding structured yet flexible storytelling. A positive first experience builds confidence and openness for future sessions.
5. Documentation, Consent and Agreements
Documentation
Being a supervisor or receiving supervision is a form of CPD, so document all your sessions!
Clinical Supervision Agreement
Most workplaces will want clinicians to have a clinical supervision agreement arranged at the first session, covering practicalities like how often you’ll meet, what you will and won’t discuss, how you’ll address any issues, confidentiality limits, and the responsibilities of both supervisor and supervisee.
Consent
In my practice, I provide extensive supervision and mentorship for many senior clinicians without formal clinical supervision agreements. Instead, I use a general consent form, including terms and conditions, which we discuss and sign together.
6. Apply Reflective Models
Using a reflective model helps ensure that supervision remains evidence-based and centred on open, respectful questioning rather than ticking boxes. Here are two of my go-to frameworks:
- John’s Model of Reflection
- Gibbs Reflective Cycle
7. Review and Reflect Every 3–6 Months
A review session is an excellent opportunity for supervisees to reflect on their learning achievements and goals, and for supervisors and supervisees to exchange feedback. Reviews should be strength-based and guided by accessible tools — for example, I use resources from the Australian College of Nurse Practitioners (2015).
Supervisors and supervisees might also create a personalised review tool during their initial session.
What to Expect in Supervision
Supervision should allow supervisees to discuss anything impacting their work life, including personal matters. Supervisors must be prepared for whatever arises, stay aware of their triggers, and manage them professionally.
Confidentiality must be upheld unless a supervisee is at risk of harm to themselves or others, in which case confidentiality may be breached with transparency. Supervisors should also suggest helpful resources if they identify additional supports that may benefit the supervisee.
Creating Safe Spaces for Storytelling and Supervision
Most people have had an experience where they felt fragile and then took the courage to speak about how they felt with a loved one who they felt would nurture them at the time. Sometimes, the opposite happens, and you walk out feeling worse than when you started and regret ever opening your mouth.
Based on the 1973 Bruskin survey fears list reported in Spectra (Speech Communication Association, 1973), their findings indicated that death was not one of the top contenders for the biggest fears. Instead, speaking before a group is the fear most selected and, thus, the most common fear (Dwyer, 2012).
When it comes to supervision, creating a safe environment is essential.
Ground Rules
People need to be in a safe place to open up. Whether it's one-on-one or group supervision, discuss ground rules together to help support this. Making fair ground rules encourages storytelling. For example:
- Listen respectfully.
- De-identify patients.
- Strict confidentiality.
- Respect diverse opinions.
Choose the Right Setting
For many reasons, having a supervision session in the middle of a busy workplace is not a good idea. Find a space that feels neutral and refreshing for everyone.
In my experience as a supervisor and supervisee, the best settings for supervision include:
- Walking and talking.
- Sitting at a quiet coffee shop.
- Sitting in a courtyard amongst nature.
Each person should know when the next session is scheduled at the time of supervision so they can prioritise attendance. Discourage mobile phone use during the session unless it is an emergency.
Supporting Quiet Clinicians to Share Their Stories
We must remember, too, that a lot of clinicians are quiet. Sometimes people assume they don’t have anything to say if someone isn't speaking. Quiet people often have a lot to say because they generally take in a lot of information through listening without talking. I’ve learned that all people want a chance to tell their story, just with the right people and in the right forum, without feeling pressured - clinical supervisors can help them do that.
Creative Approaches to Storytelling
Getting creative can make supervision more relaxed, playful, and effective.
- Use sensory aids: My supervision kit includes naturally scented hand balms, a head massager, pencils and mandalas to colour in, a candle, various fidget widgets, and of course, my childhood teddy bear, Oliver, who has travelled with me all over Australia and the world.
- Invite playful check-ins: I use posters featuring different dog and cat faces to help supervisees check in with their mood. Asking, 'On a scale of dog/cat, which one are you today and why?' can open up gentle conversations, especially for quieter individuals.
- Travel companions: Objects like Oliver can act as icebreakers and connection points, reminding us that storytelling doesn't always have to be serious—it can be comforting, playful, and deeply human.
Encouraging Storytelling Beyond Spoken Word
Other ways to encourage storytelling for clinicians can include the written word, such as journaling and publications:
Journaling
Journaling offers emotional processing for busy clinicians. It may even inspire insights to bring into supervision sessions.
- During my graduate nursing year, keeping a diary helped me process experiences I couldn’t always manage during busy shifts.
- Daily 100-word exercises, like those encouraged by my grade 12 creative writing teacher, build confidence and reflection skills.
Publishing Stories
Senior nurses encouraged me to submit pieces early in my career, leading to my first articles being published.
Since then, I've written numerous articles for various journals and magazines and was even a co-author for the International Science Journal, Springer Nature.
I never thought I'd get that first article published as a junior clinician. Senior clinicians encouraged me, and that support led me not just to publish but also to become a researcher—something I hadn't imagined for myself.
Scientific articles are quite different from opinion pieces: scientific writing tends to be more rigid, finicky, and reviewed by those who are, frankly, a little anally retentive. I prefer a less academic style, but developing confidence in both worlds has been empowering.
So my top tips:
- Start small: Internal newsletters or short stories are a great place to start.
- Mentorship is key: Encouraging others makes all the difference to confidence.
I’ve learned that with the right support, if your heart's in it and you are willing to do the work, so much is possible.
In Summary (Because Otherwise I Will Write All Day)
Years ago, a friend encouraged me to write a book capturing nursing stories — and over several years, I did. I wanted to tell nursing stories honestly: the heartwarming, heartbreaking, strange, spiritual, political, controversial, and funny. Publishing was not easy, but I realised the significance lay not in fame or uniqueness, but in sharing collective experiences from the healthcare frontline.
Readers inside and outside healthcare have told me the stories resonated with them — a reminder that storytelling binds us, connecting emotions even across different life experiences. That is the power of empathy.
Anything of true value involves vulnerability. Through storytelling and supervision, I’ve learned that while sharing honestly can feel scary, it has a far greater positive impact than we often realise. Being a storyteller and a listener is an act of courage, growth, and connection.
References
- What is Narrative Therapy?
- Quick facts: Dialectical behaviour therapy (SANE Australia, 2017)
- How Effective is Clinical Supervision? (Australian Clinical Supervision Association, 2024)
- John Model of Reflection (2020)
- Gibbs Reflective Cycle (2023)
- Australian College of Nurse Practitioners (ACNP)
- Is Public Speaking Really More Feared Than Death? (2012)
Author

Rasa Kabaila
Rasa Kabaila is a Nurse Practitioner specialising in mental health and the founder of Broadleaf HNP Services. Her approach is innovative, holistic, individualised, and evidence-based, with a strong focus on recovery-oriented care. Deeply empathetic and passionate about helping others, Rasa began her healthcare career as a personal care worker at just sixteen.
She has successfully implemented research-backed clinical therapies for optimising the treatment of anxiety and depression, including pet therapy. Beyond her clinical work, Rasa has volunteered on nursing expeditions overseas and completed Ashtanga Yoga training in Mysore, India.
Rasa is also a Conjoint Lecturer with UNSW Rural Medical School and has been an academic tutor for undergraduate nurses and paramedics at the Australian Catholic University and the University of Canberra.
Her first book, Put Some Concrete in Your Breakfast: Tales from Contemporary Nursing, was published by Springer Nature in March 2023 and has since been read by over 17,000 readers. It has also been widely promoted across journals, magazines, and news channels.
For more about Rasa’s work, visit her practice website at Broadleaf HNP Services or explore her book, Put Some Concrete in Your Breakfast: Tales from Contemporary Nursing, featured on ABC News, available on Amazon and Goodreads.



