Nurses are constantly on their feet.
Besides back pain, one of the most common painful conditions that plague nurses is foot pain. While back pain can be particularly difficult to treat, foot pain isn’t that easy either.
It seems like nurses are constantly looking for the perfect pair of shoes or inserts to make their shifts as well-cushioned as possible. Some swear by certain brands of shoes, while others use compression stockings to help ease aching feet.
One of the most common causes of foot pain, found often in athletes, is plantar fasciitis - though you don’t have to exercise to acquire this ailment. Contributors can include obesity or regularly wearing shoes with inadequate support.
Plantar fasciitis can cause crippling pain, and once you have it, it seems that no shoes or stockings are going to help.
What is Plantar Fasciitis?
Plantar fasciitis is an overuse injury like carpal tunnel syndrome (Zelman & Frysh 2023).
Commonly presenting as a stabbing pain in the sole of the foot (Mayo Clinic 2023), plantar fasciitis is a much more complex beast than it seems on paper.
While other overuse injuries result from the thickening or degeneration of tendons, plantar fasciitis does not. The plantar fascia is not a tendon - it’s a sheet of connective tissue, more similar in structure to a ligament (Esperance Podiatry 2023).
The plantar fascia originates in the medial tubercle of the calcaneus, runs the length of the foot, spanning the arch, and then terminates into the transverse ligaments of the metatarsal heads (Young 2023).
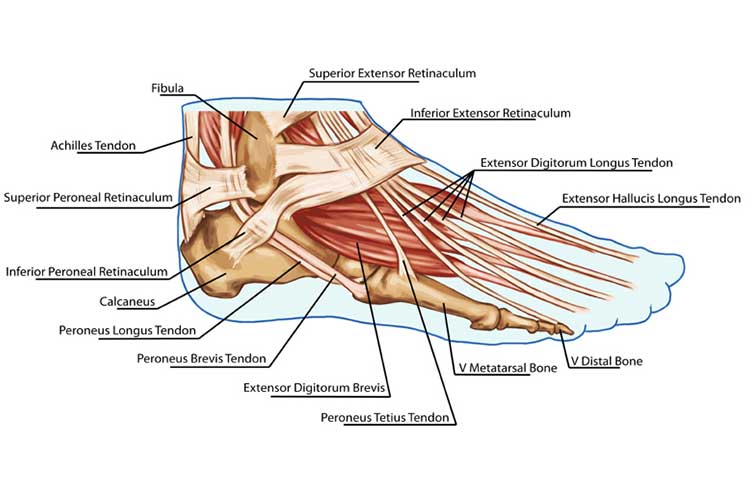
Essentially this means that the thick, fibrous ligament spans from the heel to just in front of the toes. It acts as a cantilever for the arch.
When walking puts pressure on the arch, the ligament stretches. The pressure then comes off the arch with retraction, and the plantar fasciitis snaps back to keep the arch from collapsing (The StayWell Company 2022).
The problem arises when the ligament is overused. The insertion point can easily cause small tears in the plantar fascia, which cause pain, inflammation and tenderness (Young 2023).
Many people mistake the tears for heel spurs because of where the pain originates, but the fact is that you can have heel pain from plantar fasciitis without a spur. Similarly, a spur may be present that has nothing to do with the heel pain (Healthdirect 2023).
‘Degenerative fasciosis without inflammation' is probably the most accurate way to describe plantar fasciitis. The fascia on the plantar surface of the foot is dying - it’s necrotic - and that’s why it hurts (Young 2023).
This sounds extreme, but this death is at a cellular level. Plantar fasciitis is the loss of healthy connective tissue and the development of scar tissue. Understanding this is key to treating it.
Preventing Plantar Fasciitis
Plantar fasciitis is very common in runners, which means that a certain amount of repetitive trauma may be the cause of the tears (Young 2023).
The shoes nurses wear are absolutely critical to preventing plantar fasciitis and saving themselves a great deal of pain.
Firstly, you want a cushioned heel to prevent repetitive stress on the insertion point of the plantar fascia. This can help prevent microtears (Healthdirect 2023).
Secondly, you should have proper heel support built into the shoe. You will also want to have solid arch support, especially if you have flat feet. The constant downward pressure of the weight on the arch can also cause tears, and having the arch supported prevents these from occurring (Healthdirect 2023).
If your shoes do not have these features, you can use orthotics to prevent plantar fasciitis. Orthotics are inserts that are put in the shoe to provide support (Healthdirect 2023).

Plantar Fasciitis Treatment: What Works?
There are many treatment options available for plantar foot pain, all with varying effectiveness, but efficacy is not the only factor you should consider.
Different medications and procedures will work with different patient outlooks, volumes of function and recovery times. Some options simply mask symptoms, which might be okay for some, while other treatments are more curative and will address the problem at its root.
Medical Treatments for Plantar Fasciitis
Sometimes, no matter how careful you are or how supportive the shoe is, you might still manage to tear your plantar fascia. There are a number of options that may be considered in treating plantar fasciitis:
Non-steroidal anti-inflammatory medicines (NSAIDs)
NSAIDs are used to manage almost any condition that causes symptomatic pain. One of the most commonly known NSAIDs is ibuprofen.
NSAIDs are not a solution to plantar foot pain, but they are likely to provide some relief (Mayo Clinic 2023). It is important to remember that plantar fasciitis is not actually caused by inflammation - this is only a symptom.
Corticosteroid injection
Corticosteroid injections are another method of pain reduction - not a treatment. They involve directly injecting synthetic cortisone into the plantar fascia (Young 2023).
Cortisone is a powerful anti-inflammatory substance that can act to reduce pain in the area, but as mentioned, inflammation is not the source of plantar fasciitis (Young 2023).
Platelet-rich plasma injections (PRP)
Platelet activation plays a key role in tissue healing throughout the body, and the repair of the plantar fascia is no exception.
PRPs are composed of a portion of the patient’s own blood, extracted and modified so that the platelet concentration within it is above baseline (OrthoInfo 2022).
When injected into regions of injury such as tendons, ligaments, muscles and joints, increased platelet concentration can be directly linked to improved function and decreased pain in the treated area (Penn Medicine 2021).
Side effects of these injections are often limited as the patient is utilising their own blood (Penn Medicine 2021).
PRPs are not enough to be curative in and of themselves, and it’s important to follow a program of rest, progressive stretching and strengthening to complement the procedure.
Surgical Interventions
Surgical interventions are a more invasive measure, with extended recovery times and, as with all surgery, the added risks of potential infections and complications.
Surgery
Surgery is usually the last resort for severe, debilitating plantar fasciitis pain (Young 2023).
Very rarely is surgery needed to release the plantar fascia (Healthdirect 2023).
Therapies
Therapies are likely to be your best option when it comes to addressing plantar fasciitis. These are not as extreme as surgery, nor are they simply treating the symptoms. Physical therapies address the root of the problem.
Stay off your feet for a few days, avoid high-impact activities, and give it some time. It might seem frustrating to wait around and do nothing, but that time spent taking it easy can be a huge investment in a foot-pain-free future.
Physical therapy
Exercises to stretch and strengthen the plantar fascia, Achilles tendon, and lower leg muscles may be helpful in treating plantar fasciitis (Mayo Clinic 2023).
Physical therapists might also offer massage, contrast baths or ultrasonography to help with long-term healing (Young 2023).
Other Interventions for Plantar Fasciitis
Orthotics: Arch support and heel cups
Orthotics, which are placed inside the shoes and provide extra support for the arch of the foot, are (theoretically) perfect for preventing plantar foot pain and are often the first line of treatment.
Strain is placed on your plantar fascia to keep the shape of your heel arch. So, if you can place something under your foot to keep it in a neutral arch position, you’ll be putting less strain on the fascia.
Splints
Splints are the next line of treatment. These devices hold your foot at a flexed angle to relieve the pressure on the tears. They are usually worn at night (Young 2023).
Conclusion
There are many options available to assist you if you suffer from plantar foot pain, but only a limited number should be labelled as treatments.
The best options are to avoid symptom masking and work on resting and addressing the over-strained plantar fascia naturally.
Topics
References
- Esperance Podiatry 2023, ‘The Structure and Function of the Plantar Fascia’, Esperance Podiatry Blog, 11 March, viewed 16 July 2024, https://www.esperancepodiatry.com.au/blog/plantarfascia-structure-and-function
- Healthdirect 2023, Plantar Fasciitis, Australian Government, viewed 16 July 2024, https://www.healthdirect.gov.au/plantar-fasciitis
- Mayo Clinic 2023, Plantar Fasciitis, Mayo Clinic, viewed 16 July 2024, https://www.mayoclinic.org/diseases-conditions/plantar-fasciitis/symptoms-causes/syc-20354846
- OrthoInfo 2022, Platelet-Rich Plasma (PRP), OrthoInfo, viewed 16 July 2024, https://orthoinfo.aaos.org/en/treatment/platelet-rich-plasma-prp/
- Penn Medicine 2021, Platelet Rich Plasma Treatment, The University of Pennsylvania, viewed 16 July 2024, https://www.pennmedicine.org/for-patients-and-visitors/find-a-program-or-service/orthopaedics/programs-and-centers/regenerative-sports-medicine/platelet-rich-plasma-treatment
- The StayWell Company 2022, Plantar Fasciitis, Cedars-Sinai, viewed 16 July 2024, https://www.cedars-sinai.org/health-library/diseases-and-conditions/p/plantar-fasciitis.html
- Young, C 2023, Plantar Fasciitis, Medscape, viewed 16 July 2024, https://emedicine.medscape.com/article/86143-overview?form=fpf
- Zelman, D & Frysh, P 2023, Guide to Overuse Injuries, WebMD, viewed 16 July 2024, https://www.webmd.com/pain-management/ss/slideshow-overuse-injuries
 New
New 
