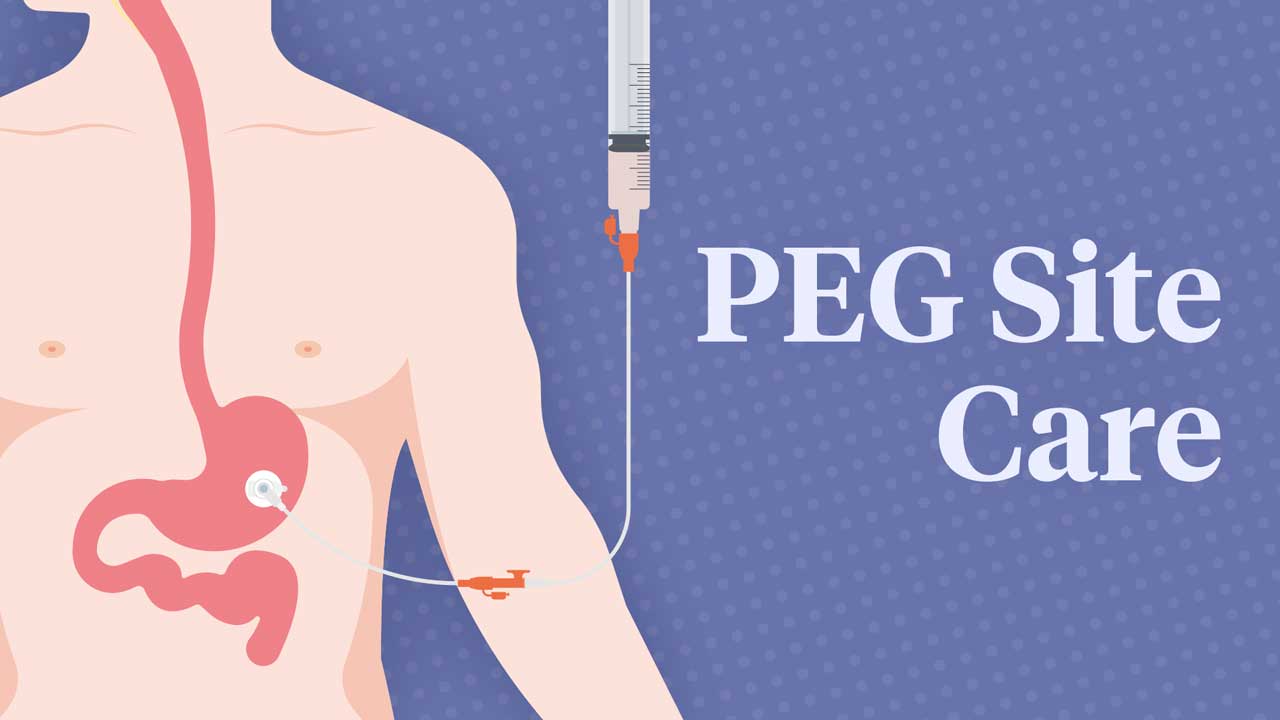
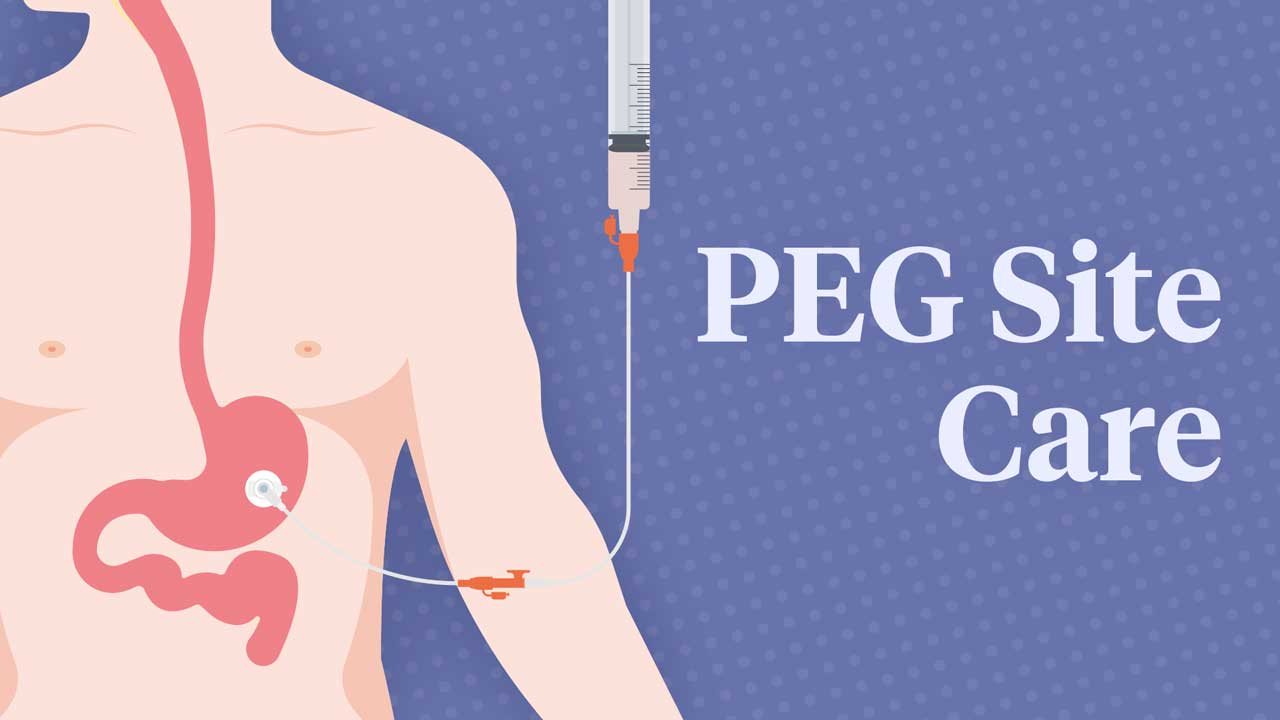
A percutaneous endoscopic gastrostomy (PEG) tube is a feeding tube that is inserted into the stomach via a surgical incision in the abdomen (known as a stoma). A PEG may be inserted if a person is unable to safely eat and drink through their mouth (Healthdirect 2024).
When caring for someone with a PEG tube in situ, you should be able to perform basic personal care of the stoma site and identify any red flags that require an escalation of care.
Monitoring the PEG Site
Routine care should comprise:
- Making sure that the PEG tube is properly supported and secured
- Making sure that the external flange is 2 to 5 mm from skin level, and adjusting this if required
- Checking for any signs of tube migration and escalating care if necessary.
(ACI & GENCA 2015)
Performing Personal Care of the PEG Site
- The skin around the insertion site and under the plastic flange should be cleaned at least two to three times daily. Use a clean cloth and tap water. If you have any concerns about possible infections or other issues, escalate to your line manager.
- Start with cleaning as part of the client’s daily shower routine.
- The PEG tube should be rotated completely (360 degrees) once per day (starting three to five days after insertion). Refer to the client’s care plan instructions.
- Dressings should not be placed under the flange unless instructed to do so or if there is leakage (until reviewed by a clinician).
- Ensure the client maintains adequate oral hygiene.
- Place the clamp on the tube in a new position each day to prevent it from weakening.
- Note that it’s normal for the client to experience redness, crustiness and moistness around the insertion site.
- Escalate to an appropriately qualified medical practitioner if the client is concerned about tenderness around the insertion site.
(RCHM 2021, 2024)
How to Clean the PEG Site
- Explain the procedure to the client and obtain consent.
- Ensure the client’s privacy and comfort.
- Perform hand hygiene.
- Gather all equipment to carry out the task (e.g. a bowl of warm water, a cloth).
- Perform hand hygiene.
- Don appropriate PPE in accordance with your organisation’s policies and procedures.
- Clean the stoma with soap or body wash and water (alternatively, you can use saline or salty water) twice daily.
- Thoroughly dry the area around the tube and under the external bumper. This will help prevent skin breakdown.
(RCHM 2021; NEMO 2024)
When to Escalate Care
The following signs and symptoms require escalation of care to an appropriately qualified medical practitioner:
- Pain or discomfort at the stoma site
- New bleeding
- Gastric fluid leak
- Skin or stoma site complications, including
- Excoriation or breakdown of the skin
- Pressure injury
- Embedded sutures
- Infection (e.g. cellulitis, folliculitis)
- Tube displacement
- Tube deterioration
- Buried bumper syndrome (a complication that occurs months to years after the insertion date of the PEG. BBS is where the PEG's external flange migrates into the individual’s abdominal wall, which may cause a partial or complete blockage of the tube.)
- Diarrhoea
- Constipation
- Nausea
- Vomiting
- Accidental removal of the PEG tube.
(ACI & GENCA 2015; Hoang et al. 2019; SAGES 2019)
What to Do if the PEG Tube Falls Out
- Stay calm and reassure the client.
- Cover the stoma with a dressing.
- Escalate to your line manager so that an appropriately trained medical practitioner can insert a new tube as soon as possible before the stoma closes.
(RCHM n.d.; Kent Community Health NHS Foundation Trust 2022)
Note: This article is intended as a guide only for non-clinical staff providing PEG site care to home care clients and should not replace best-practice care. Always refer first to your organisation's policies and procedures on PEG site care.
Test Your Knowledge
Question 1 of 3
How much should the PEG tube be rotated daily?
Topics
References
- Agency for Clinical Innovation and the Gastroenterological Nurses College of Australia 2015, A Clinician’s Guide: Caring for People With Gastrostomy Tubes and Devices From Pre-Insertion to Ongoing Care and Removal, New South Wales Government, viewed 22 July 2025, https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0017/251063/gastrostomy_guide-web.pdf
- Healthdirect 2024, PEG Tube Placement, Australian Government, viewed 22 July 2025, https://www.healthdirect.gov.au/peg-tube-placement
- Hoang, PT, Menias CO & Niemeyer, MM 2019, ‘Percutaneous Gastrostomy Tube Placement: Recognizing When Things Go Wrong’, Semin Intervent Radiol., vol. 36, no. 3, viewed 28 July 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6699954/
- Kent Community Health NHS Foundation Trust 2022, What Do to if Your Gastrostomy Feeding Tube Comes Out, National Health Service, viewed 28 July 2025, https://www.kentcht.nhs.uk/leaflet/what-do-to-if-your-gastrostomy-feeding-tube-comes-out/
- Nutrition Education Materials Online 2024, Caring for Your Gastrostomy Tube, Queensland Government, viewed 28 July 2025, https://www.health.qld.gov.au/__data/assets/pdf_file/0025/152557/hphe-gastrostomy.pdf
- Royal Children’s Hospital Melbourne n.d., Clinical Practice Guidelines: Gastrostomy Acute Replacement of Displaced Tubes, RCHM, viewed 28 July 2025, https://www.rch.org.au/clinicalguide/guideline_index/Gastrostomy_acute_replacement_of_displaced_tubes/
- Royal Children’s Hospital Melbourne 2021, Percutaneous Endoscopic Gastrostomy (PEG) Tube Basic Care Guide, RCHM, viewed 28 July 2025, https://www.rch.org.au/uploadedFiles/Main/Content/gastro/PEG%20Basic%20care%20guide%20-%20January%202021.pdf
- Royal Children’s Hospital Melbourne 2024, Nursing Guidelines: Gastrostomy, RCHM, viewed 28 July 2025, https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Gastrostomy/#
- Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) 2019, Late PEG Complications: Recurrent Cellulitis, Leakage, Buried Bumper Syndrome, online video, 28 June, viewed 28 July 2025, https://www.youtube.com/watch?v=tyVXpiOXr5g
 New
New