Maths can be intimidating to some but being able to make quick calculations is an essential skill for healthcare practitioners.
Calculating the correct dose of any medicine you administer is crucial in avoiding medication errors. Administering the wrong dose can have severe consequences for the patient, such as preventable morbidity and even death (Tariq et al. 2023).
While miscalculation is a serious and entirely preventable adverse event, healthcare professionals are human, and errors can still occur.
We, therefore, have a responsibility to our patients to find ways of minimising instances of medication errors from occurring.
We can’t rely solely on technology. Even though devices like calculators and programmable IV pumps are convenient and helpful, we need to be able to verify calculations and have a sense of what seems right mathematically (Wilson & Miller 2013; Schnur 2021).
While the exact rates of medicine miscalculation in Australia are unknown, medicine-related problems account for 250,000 hospital admissions every year (DoHaAC 2022).
Furthermore:
- The annual cost of medicine-related hospital admissions is $1.4 billion
- Medicine-related problems likely account for 400,000 additional presentations to emergency departments
- 50% of medicine-related harm is preventable.
(DoHaAC 2022; PSA 2019)
One study, which examined medication errors made in an Australian pediatric hospital over a five-year period, found that medicine miscalculation was a factor in 341 or 5.1% of cases (Manias et al. 2018).
Numeracy skills are crucial in ensuring patient safety. However, literature suggests that undergraduate nursing students and registered nurses alike lack competency in this area (Minty-Walker et al. 2021).
This article will provide a refresher on the basics of medicine calculation.

Why Do Medicine Miscalculations Occur?
Common causes of medication errors and miscalculations include:
- Mathematical anxiety
- Distractions
- Time pressure and rushing
- Illegible writing
- Confusing symbols or abbreviations
- Misplacing or failing to write decimal points, or failing to write ‘0’ before a decimal point
- Failing to use universal measurements
- Forgetting to consider the patient’s age, which may change calculations
- Forgetting to write the duration of treatment or specifying the number of doses
- Inexperience
- Stress and fatigue.
(Sayadi et al. 2021; Tariq et al. 2023)
Fundamental Calculations
Units of Measurement
Medicines use a range of units of measurement. Knowing the differences between each unit of measurement and being able to convert one to another are essential competencies, as conversion mistakes can cause patients to receive much more or less medicine than they need, with potentially severe consequences (Wright & Shepherd 2017).
Medicines are generally measured using either:
- Weight:
- Grams (g)
- Milligrams (mg)
- Micrograms
- Nanograms
- Volume:
- Litres (L)
- Millilitres (mL)
- Standardised international units
- Strength of solution when a weight of medicine is dissolved in a volume of liquid
- Percentages.
(Wright & Shepherd 2017)
Converting Units of Measurement
The main units of measurement that healthcare practitioners will need to convert are metric weights.
An important rule to remember is that metric weights use a factor of 1,000, meaning that:
- When you convert a larger unit to a smaller unit, the bigger unit needs to be multiplied by 1,000. This can be achieved by moving 3 decimal points to the right (e.g. 5 g = 5,000 mg)
- When you convert a smaller unit to a larger unit, the smaller unit needs to be divided by 1,000. This can be achieved by moving 3 decimal points to the left (e.g. 5 g = 0.005 kg).
(Wright & Shepherd 2017; Tweedy & Mason 2000)
Note: Metric volumes also use a factor of 1,000, i.e. 1 L = 1,000 mL and 1 mL = 0.001 L.
| Kilograms | Grams | Milligrams | Micrograms | Nanograms | |
|---|---|---|---|---|---|
| Kilograms | 1 kg = 1,000 g | 1 kg = 1,000,000 mg | 1 kg = 1,000,000,000 micrograms | 1 kg = 1,000,000,000,000 nanograms | |
| Grams | 1 g = 0.001 kg | 1 g = 1,000 mg | 1 g = 1,000,000 micrograms | 1 g = 1,000,000,000 nanograms | |
| Milligrams | 1 mg = 0.000001 kg | 1 mg = 0.001 g | 1 mg = 1,000 micrograms | 1 mg = 1,000,000 nanograms | |
| Micrograms | 1 microgram = 0.000000001 kg | 1 microgram = 0.000001 g | 1 microgram = 0.001 mg | 1 microgram = 1,000 nanograms | |
| Nanograms | 1 nanogram = 0.000000000001 kg | 1 nanogram = 0.000000001 g | 1 nanogram = 0.000001 mg | 1 nanogram = 0.001 micrograms |
These conversions must be checked thoroughly to ensure the patient doesn’t receive too much or too little of their medicine. Perform the calculation twice in order to verify the result and always ask a colleague to perform the calculation themselves in order to double-check (Wright & Shepherd 2017).
Important Formulas
Calculating Tablet Dose Forms
|
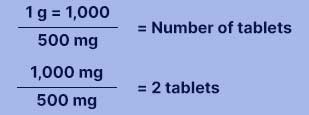
|
| Calculating Mixtures and Solutions
*This formula is not only used for intravenous medicines, but for oral medicines as well.
|
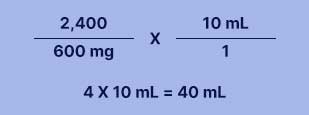
|
Calculating Intravenous Fluid Rate
|
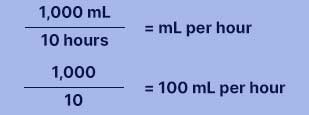
|
Calculating Millilitres Per Minute
|
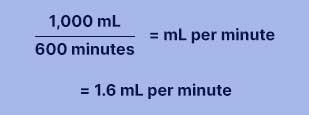
|
Calculating Drops Per Minute
|
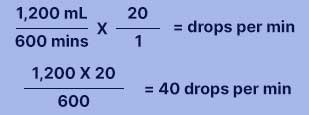
|
(SLSS 2022)
Rounding Up or Down
Sometimes a calculation will result in a number with decimals. Depending on the situation, you might need to round these numbers off to a whole number or round off to a certain number of decimal places.
When rounding off, check the first number out of all the ones you want to drop:
- If the number is 5 or more, round up
- If the number is lower than 5, round down.
(Centennial College 2024)
For example, say you want to round off the number 5.762.
- If you want to round off to a whole number, you would round up to 6.0 because the first decimal place is 7
- If you want to round off to one decimal place, you would round up to 5.8 because the second decimal place is 6
- If you want to round off to two decimal places, you would round down to 5.76 because the second decimal place is 2.
Medicine Calculation Tips

- Before making a calculation, use common sense to estimate the answer. If the number you end up with is wildly different to what you guessed, it may be a sign that you’ve miscalculated.
- Always check abbreviations. Micrograms should not be abbreviated as the abbreviation (mcg) looks too similar to milligrams (mg).
- Always have a colleague double-check your calculations.
- If you are unfamiliar with a medicine, check its usual dose and method of administration using the latest edition of either eMIMS, AusDI or the Australian Medicines Handbook.
- Complex calculations involving multiple steps and requiring several mathematical skills (different types of computations and conversions) are particularly high risk as there are several stages where an error could occur. Those that involve very small dosages are especially risky. Always check your calculation thoroughly and ask a colleague to perform the same calculation independently to ensure you administer the correct dosage.
- Avoid distractions when performing calculations
- Avoid rushing calculations.
(SLSS 2022; Wright & Shepherd 2017)
Test Your Knowledge
You can check your competency in arithmetic, conversion and calculation by taking interactive medicine calculation quizzes on the Flinders University website.
Overcoming Medicine Miscalculation
Medicine miscalculation is an issue for new and experienced health practitioners alike.
Literature suggests that a two-fold approach is important for reducing the rates of miscalculation: focusing on undergraduate mathematical skills as well as testing graduates for ongoing competence. Suggestions for undergraduates include practical sessions and assessments in safe environments that can aid the hands-on learner, and assisting them to gain confidence as practitioners. Remedial help should be available for those who require it.
Despite numerical competency tests being perceived as 'highly stressful and exceptionally challenging' by healthcare professionals (Bayne & Bindler 1997), it’s been argued that regular testing using a recognised, validated and reliable assessment tool be used as a means of maintaining numeracy skills (Warburton 2010).
Furthermore, a 2021 study found that a medicine calculation training program was beneficial in reducing mathematical anxiety and improving calculation skills among students. It suggested that introducing similar programs in nursing schools would be beneficial in reducing the risk of miscalculation (Sayadi et al. 2021).
Raising awareness of medicine miscalculations within the healthcare population can be achieved by regularly monitoring and reporting these errors. Practitioners can be involved in assessing the cause of the problem and can make suggestions on how to avoid future errors.
Conclusion
Using calculators and conversion charts may be helpful, but should never be used as a substitute for taking into consideration the logical or expected answer. Unfortunately, today's busy healthcare environments mean that all too often, we’re rushing to complete tasks efficiently.
It’s important to nurture an environment where you and your colleagues feel supported in medical calculations, even if you occasionally make errors. Discussing the error in a supportive manner will go a long way in encouraging struggling practitioners to persevere and achieve better calculation results in the long term.

Test Your Knowledge
Question 1 of 5
Which one of the following is equal to 24 g?
Topics
References
- Bayne, T & Bindler, R 1997, ‘Effectiveness of Medication Calculation Enhancement Methods with Nurses’, JNSD: Journal of Nursing Staff Development, vol. 13, no. 6, pp. 293-301, viewed 23 November 2016, https://pubmed.ncbi.nlm.nih.gov/9429370/
- Centennial College 2024, General Dosage Rounding Rules, Centennial College, https://libraryguides.centennialcollege.ca/c.php?g=645085&p=5268478
- Department of Health and Aged Care 2022, Guiding Principles for Medication Management in the Community Collection, Australian Government, viewed 15 January 2024, https://www.health.gov.au/resources/collections/guiding-principles-for-medication-management-in-the-community-collection
- Manias et al. 2018, ‘Medication Error Trends and Effects of Person-Related, Environment-Related and Communication-Related Factors on Medication Errors in a Paediatric Hospital’, Journal of Paediatrics and Child Health, vol,. 55, no. 3, viewed 15 January 2024, https://onlinelibrary.wiley.com/doi/full/10.1111/jpc.14193
- Minty-Walker, C, Wilson, N J, Rylands, L, Hunt, L & Pettigrew, J 2021, ‘Undergraduate Nursing Curricula: Numeracy and Accreditation’, Collegian, vol. 28, no. 5, viewed 15 January 2024, https://www.collegianjournal.com/article/S1322-7696(20)30142-6/fulltext
- Pharmaceutical Society of Australia 2019, Medicine Safety: Take Care, PSA, viewed 15 January 2024, https://www.psa.org.au/wp-content/uploads/2019/01/PSA-Medicine-Safety-Report.pdf
- Sayadi, L, Nasrabadi, AN & Hosseini, A 2021, ‘The Effect of Drug Dosage Calculation Training Program on Math Anxiety and Nursing Students’ Skills: A Non-Randomized Trial Study’, Nursing Practice Today, vol. 8, no. 3, viewed 15 January 2024, https://npt.tums.ac.ir/index.php/npt/article/view/1156
- Schnur, MB 2021, ‘Drug Calculations: How to Use the Universal Formula’, NursingCenter Blog, 23 July, viewed 15 January 2024, https://www.nursingcenter.com/ncblog/july-2021/drug-calculations-universal-formula
- Student Learning Support Service 2022, Drug Calculations, Flinders University, viewed 15 January 2024, https://students.flinders.edu.au/content/dam/student/slss/numeracy/drug-calcs.pdf
- Tariq, RA, Vashisht, R, Sinha, A & Scherbak, Y 2023, ‘Medication Dispensing Errors And Prevention’, StatPearls, viewed 15 January 2024, https://www.ncbi.nlm.nih.gov/books/NBK519065/#article-24883.s2
- Tweedy, J & Mason, D 2000, Drug Calculations, Canterbury District Health Board, viewed 15 January 2024, https://edu.cdhb.health.nz/Hospitals-Services/Health-Professionals/pdu/Documents/Clinical%20Calcs%20Revision%20Package.pdf
- Warburton, P 2010, ‘Numeracy and Patient Safety: The Need for Regular Staff Assessment’, Nursing Standard, vol. 24, no. 27, viewed 20 January 2022, https://journals.rcni.com/nursing-standard/numeracy-and-patient-safety-the-need-for-regular-staff-assessment-ns2010.03.24.27.42.c7620
- Wilson & Miller, K 2013, ‘The Nurse's Quick Guide to I.V. Drug Calculations’, Nursing Made Incredibly Easy!, vol. 11, no. 2, viewed 15 January 2024, https://journals.lww.com/nursingmadeincrediblyeasy/fulltext/2013/03000/the_nurse_s_quick_guide_to_i_v__drug_calculations.1.aspx
- Wright, K & Shepherd, E 2017, ‘How to Calculate Drug Doses and Infusion Rate Accurately’, Nursing Practice, vol. 113, no. 11, viewed 15 January 2024, https://cdn.ps.emap.com/wp-content/uploads/sites/3/2017/10/181017-How-to-calculate-drug-doses-and-infusion-rates-accurately.pdf
Additional Resources
- Recommendations for Terminology, Abbreviations and Symbols Used in Medicines Documentation | ACSQHC
- Basic Drug Calculations: Check Your Competency | Flinders University
- Drug Calculations | Flinders University
- Medication Safety | Ausmed Course
- Preventing Medication Errors | Ausmed Course
- Aged Care: Medication Management and Error-Reduction | Ausmed Lecture
 New
New