Alcohol and drug consumption (both legal and illegal) are a leading cause of preventable harm in Australia (AIHW 2025).
The use of alcohol and drugs is associated with a variety of adverse health, social and economic effects, including:
- Decreased workplace productivity
- Relationship issues or family breakdown
- Increased healthcare and law enforcement costs
- The perpetuation of marginalisation and disadvantage
- Social isolation
- Unemployment
- Homelessness and poverty
- Impaired childhood development or trauma
- Criminal prosecution
- Violence and crime
- Motor vehicle accidents
- Injury
- Disease
- Mental illness
- Pregnancy complications
- Harm related to injections
- Overdose
- Mortality.
(DoHaAC 2023; Better Health Channel 2019; AIHW 2025; NCETA 2024)
Despite this, 1 in 4 Australians are consuming alcohol at levels considered risky (DoHaAC 2023), and about 1 in 20 Australians are experiencing addiction or substance abuse (Healthdirect 2023).
There is no level of alcohol or drug use that is completely safe. However, there are ways to reduce the risk of harm (ADF 2023).
The Three Pillars of Harm Minimisation
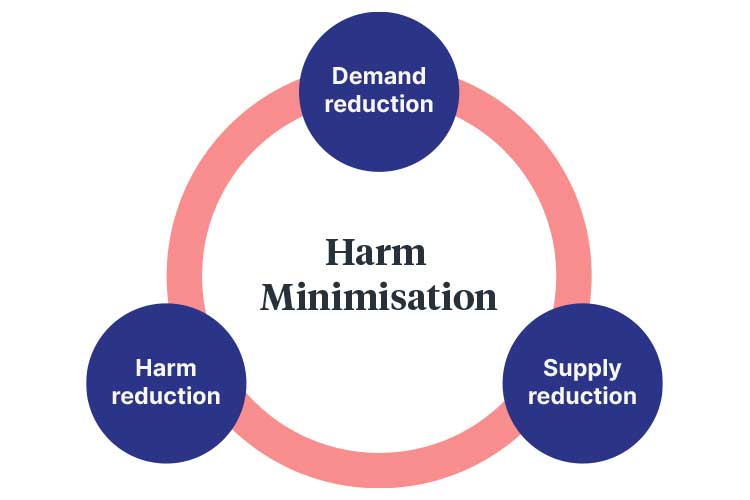
Australia’s National Drug Strategy is guided by three pillars of harm minimisation. They are:
- Demand Reduction, which involves preventing and/or delaying alcohol and drug use, reducing the misuse of alcohol and drugs, and using evidence-informed treatment to support recovery from dependence.
- Supply Reduction, which involves reducing the production and supply of illicit drugs and regulating the supply of legal drugs.
- Harm Reduction, which involves reducing the risk of adverse alcohol and drug-related consequences.
(DoHaAC 2023)
What is Harm Reduction?
Despite the known dangers of alcohol and drugs, some people are unable or unwilling to stop using them in risky ways (ADF 2023).
Harm reduction aims to combat this issue by decreasing the risk of negative effects associated with ongoing alcohol and drug use (Better Health Channel 2019).
The practice of harm reduction originated during the 1980s HIV epidemic, where healthcare workers attempted to reduce the spread of the virus by providing injection drug users with unused syringes (ADF 2023).
According to Harm Reduction International (2025), harm reduction describes ‘policies, programs and practices that aim to minimise negative health, social and legal impacts associated with drug use, drug policies and drug laws’.
Harm reduction is not about preventing people from using alcohol or drugs, nor does it condone alcohol and drug use. Instead, it acknowledges the risks associated with alcohol and drugs, with the aim of preventing harm to both the individual and the greater community as much as possible (ADF 2023; NCETA 2024).
Harm reduction includes interventions such as establishing safe environments for drug use, training healthcare workers to assist with and treat drug-related incidents, and providing education programs (ADF 2019a).
Priority Substances
Australia’s National Drug Strategy 2017–2026 identifies the following substances as posing an increased risk of harm to individuals and the community:
- Alcohol
- Tobacco
- Cannabis
- Methamphetamines and other stimulants
- Opioids (e.g. heroin)
- Pharmaceuticals such as opioids, benzodiazepines and analgesics being used for non-medical reasons
- New psychoactive substances such as synthetic cannabis, mephedrone and methylenedioxypyrovalerone.
(DoHaAC 2025)
Priority Populations
The National Alcohol Strategy 2019–2028 and National Drug Strategy 2017–2026 also identify specific groups of people as being at higher risk of disproportionate harm from alcohol and drugs. These groups include:
- Aboriginal and Torres Strait Islander people
- People with comorbidities such as mental illness, heart disease, diabetes, cognitive impairment and chronic pain
- Young people aged between 10 and 24
- Adults in their 40s, 50s or 60s
- Older adults aged over 60
- People in contact with the criminal justice system
- Culturally and linguistically diverse populations
- Members of the LGBTIQ+ community
- People living in remote areas
- People who are pregnant or planning a pregnancy
- People with diagnosed or suspected fetal alcohol spectrum disorder
- People whose parents or guardians are experiencing alcohol dependence.
(DoHaAC 2023, 2025)
Examples of Harm Reduction Strategies in Australia

- Needle and syringe programs, which enable injection drug users to access sterile injecting equipment
- Opioid pharmacotherapy treatment (medicinal treatment for opioid dependence)
- Peer education programs
- Drug diversion programs, which offer treatment to illicit drug users and aim to help them avoid a criminal record
- Supervised injection rooms
- Outreach services
- Sobering-up services, which provide an area for intoxicated people to withdraw safely and receive care if needed
- Testing for infections (e.g. HIV, viral hepatitis, STIs) and subsequent discussion and counselling
- Referral to treatment programs
- Overdose prevention activities such as first aid training
- Access to primary healthcare.
(Better Health Channel 2019; NCETA 2024; HRVIC 2018)
Working With Clients
When implementing harm reduction strategies with a client, it is important to keep the following principles in mind:
- Be sensitive to the client’s age, stage of life, disadvantages (if applicable) and settings of use
- Do no harm
- Focus on potential harms to the client rather than the fact that they use alcohol and/or drugs
- Focus on optimising the client’s quality of life rather than cessation
- Maximise potential intervention options
- Ensure any goals made are appropriate, practical and achievable
- Always respect the client’s rights
- Be non-judgmental in your interactions and treat all clients with dignity, compassion and respect
- Use evidence-based and cost-effective interventions
- Allow clients to actively and meaningfully participate
- Acknowledge social determinants such as poverty, social inequality and discrimination that may increase the client’s risk of harm
- Empower the client.
(YouthAOD Toolbox 2018; HRVIC 2018)
It is also important to remember that every client is different. Some people may use alcohol and drugs more frequently than others, and the potential risks will depend on the type of substance being used and the pattern in which it is being used. Therefore, multifaceted interventions are required (NCETA 2024).
Management of a Client Who is Upset or Aggressive

Alcohol and drugs interrupt normal brain function and may cause aggressive behaviour in some cases. A client may be impulsive, irritable or have difficulty assessing situations (ADF 2024).
When managing a client who is affected by alcohol or drugs and acting aggressively, it is important to know how to address the situation (ADF 2024).
1. Assess the Risks
You should consider:
- Behavioural triggers such as feeling threatened, unwelcome, judged, impatient, ignored or excluded
- The environment you are in (e.g. whether children are nearby, where exit routes are located)
- The type of substance being taken by the client, if known.
(ADF 2024)
2. Prevent Escalation
- Stay calm:
- Move slowly and avoid prolonged eye contact
- Give the client space
- Use a low, calm and steady tone when speaking
- Remove any dangerous objects
- Avoid asking too many questions
- Say ‘I am not angry with you – I just want to make sure you are safe’
- Use the client’s name when speaking to them
- Reassure the client:
- Be supportive and tell the client that they will be okay
- Move the client to a quiet area if possible
- Listen to the client and respond in a calm manner
- Avoid arguing
- Call emergency services (police, ambulance etc.) if you have any concerns for the client or yourself
- After conflict:
- Stay alert
- Keep the client calm
- Ensure others are safe
- Avoid mentioning the incident unless the client wishes to discuss it.
(ADF 2024)
Test Your Knowledge
Question 1 of 3
When responding to a client who is affected by drugs and is upset or aggressive, which one of the following actions is recommended?
Topics
References
- Alcohol and Drug Foundation 2023a, Reducing the Risk, Alcohol and Drug Foundation, viewed 11 April 2025, https://adf.org.au/reducing-risk/
- Alcohol and Drug Foundation 2024, Responding to Someone Who is Upset or Aggressive, Alcohol and Drug Foundation, viewed 11 April 2025, https://adf.org.au/reducing-risk/dealing-bad-reaction/
- Australian Institute of Health and Welfare 2020, Alcohol, Tobacco & Other Drugs in Australia, Australian Government, viewed 11 April 2025, https://www.aihw.gov.au/reports/alcohol/alcohol-tobacco-other-drugs-australia/contents/about
- Better Health Channel 2019, Reducing Harm from Alcohol and Other Drug Use, Victoria State Government, viewed 11 April 2025, https://www.betterhealth.vic.gov.au/health/ServicesAndSupport/reducing-harm-from-alcohol-and-drug-use
- Department of Health and Aged Care 2023, National Alcohol Strategy 2019–2028, Australian Government, viewed 11 April 2025, https://www.health.gov.au/resources/publications/national-alcohol-strategy-2019-2028?language=en
- Department of Health and Aged Care 2025, National Drug Strategy 2017–2026, Australian Government, viewed 11 April 2025, https://www.health.gov.au/resources/publications/national-drug-strategy-2017-2026?language=en
- Harm Reduction International 2025, What is Harm Reduction?, Harm Reduction International, viewed 11 April 2025, https://www.hri.global/what-is-harm-reduction
- Harm Reduction Victoria 2018, What is Harm Reduction?, HRVIC, viewed 11 April 2025, https://www.hrvic.org.au/what-is-harm-reduction
- Healthdirect 2023, Substance Abuse, Australian Government, viewed 11 April 2025, https://www.healthdirect.gov.au/substance-abuse
- National Centre for Education and Training on Addiction 2024, Harm Minimisation, Flinders University, viewed 11 April 2025, https://nceta.flinders.edu.au/about-aod/community/harm-minimisation
- YouthAOD Toolbox 2018, Harm Minimisation, The Centre for YouthAOD Practice Development, viewed 11 April 2025, https://www.youthaodtoolbox.org.au/harm-minimisation
Additional Resources
- Drugs contacts: A list of organisations, websites and services that offer support, counselling and information about drugs.
- Alcohol and Drug Foundation
- Harm Reduction International
- National Alcohol Strategy 2019–2028
- National Drug Strategy 2017–2026
 New
New 
