General awareness of motor neurone disease (MND) rose quickly after the Ice Bucket Challenge went viral in 2014.
How has the management of this condition advanced since then?
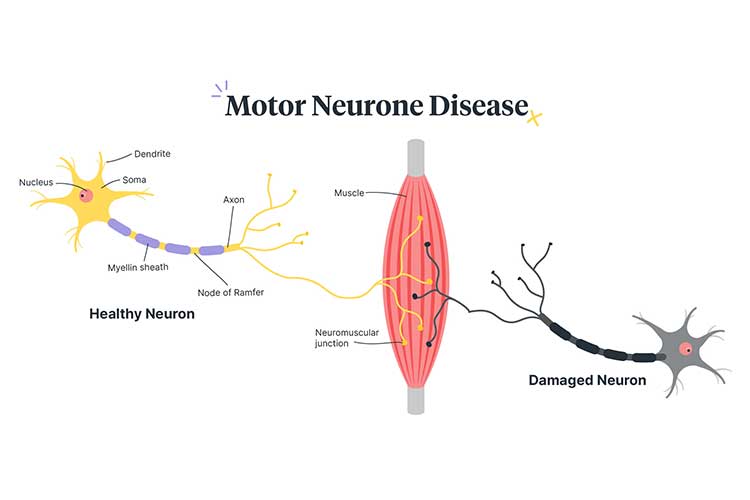
The term MND refers to a group of progressive neurological diseases that attack motor neurons in the body, eventually causing the muscles to waste away (Healthdirect 2022; QBI 2023).
To date, there is no known cure or effective treatment for MND. There are around 2,000 Australians living with MND, and 2 people die from the disease every day (QBI 2019).
MND causes simple limb movements, swallowing, talking, and even breathing to become increasingly difficult (Better Health Channel 2021).
What Causes Motor Neurone Disease?
The cause of MND remains relatively unknown.
Researchers have found that hereditary factors account for around 5 to 10% of cases, but most cases remain unidentified. Current research into this area is looking at not only genetic factors, but also nerve growth factors, the repair and ageing of motor neurons, and immune-mediated damage, as well as viruses, toxins, and chemical interactions with nerve cell control and communication (Better Health Channel 2021).
Risk Factors for Motor Neurone Disease
MND affects both adults and children. In children, MND is often genetic, and the symptoms are usually present at birth or appear in early childhood. In adults, the symptoms often appear after the age of 50 (NINDS 2020). It appears to be more common in males than in females (QBI 2019).
Symptoms of Motor Neurone Disease
MND is a progressive condition that gradually worsens. Symptoms may begin unilaterally before spreading (Healthdirect 2022).
Symptoms might include:
- Aching, cramping or twitching muscles
- Clumsiness and stumbling
- Weakness in the arms, legs, hands and voice
- Slurred speech
- Difficulty chewing and swallowing
- Fatigue
- Muscle wastage
- Weight loss
- Emotional lability (exaggerated mood changes)
- Respiratory issues.
(Better Health Channel 2021)
Complications of Motor Neuron Disease
The average life expectancy of someone with MND is 27 months from diagnosis (QBI 2019). In addition to physical symptoms, up to 50% of people living with MND will also display changes in their cognition, language, behaviour and personality as the disease progresses (Better Health Channel 2021).
Due to the physical effects of MND, patients may become dependent on others for all aspects of their day-to-day life - from mobility to eating (Better Health Channel 2021).
People with MND may also experience pain, constipation, pressure injuries, psychological distress and other difficulties (Leeds Teaching Hospitals NHS Trust n.d.).
The most common cause of death among people with MND is respiratory failure (MND Australia 2021a).
Diagnosing Motor Neuron Disease
There is no single diagnostic test for MND, but a combination of the following may be used:
- Electromyography (EMG)
- Nerve conduction studies
- MRI scan
- Blood tests
- Lumbar puncture
- Muscle biopsy.
(MND Australia 2021b)
The Nurse’s Role
The nurse’s role becomes increasingly important as MND progresses and patients may require increasing support and assistance for their day-to-day activities. The nurse will also be a member of the interprofessional team caring for the person if the individual is hospitalised.
As a nurse, you will need to be aware of the potential complications of the disease’s progression - such as aspiration - and ensure care is targeted to prevent these complications from eventuating. This could be as simple as ensuring the patient is sitting upright when eating.
The carers of those with MND may struggle with the physical and emotional demands and stress from their role, so be considerate to the needs of carers and support them during the disease’s progression.
Treatment of Motor Neuron Disease
Although MND is currently incurable, some medicines are effective in helping patients remain in the milder stages of the disease for longer, possibly prolonging their survival by two to three months. Symptoms can also be managed with the help of an interprofessional healthcare team who assists with interventions to improve quality of life during the disease’s progression (QBI 2023).
Current Research

Current research focuses on a multitude of areas within MND - from what causes it, to how to treat it. Funding is essential to ensure this research continues.
No doubt we’ve all heard about - or perhaps even participated in - the Ice Bucket Challenge. This particular initiative raised more than $115 million dollars (USD) for MND worldwide in 2014. Research funded by this campaign has already led to the identification of the gene NEK1, which is associated with about 3% of MND cases (Rogers 2016).
Test Your Knowledge
Question 1 of 3
True or false: Most cases of motor neurone disease have no identified cause.
Topics
References
- Better Health Channel 2021, Motor Neurone Disease (MND), Victoria State Government, viewed 3 October 2023, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/motor-neurone-disease
- Healthdirect 2022, Motor Neurone Disease (MND), Australian Government, viewed 3 October 2023, https://www.healthdirect.gov.au/motor-neurone-disease-mnd
- Leeds Teaching Hospitals NHS Trust n.d., How Symptoms of MND Are Managed, National Health Service, viewed 3 October 2023, https://www.leedsth.nhs.uk/a-z-of-services/leeds-motor-neurone-disease-mnd-care-centre/your-condition-and-treatment/how-symptoms-of-mnd-are-managed/
- MND Australia 2021b, Diagnosing MND, MND Australia, viewed 3 October 2023, https://www.mndaustralia.org.au/mnd-connect/for-health-professionals-service-providers/diagnosing-mnd
- MND Australia 2021a, Supporting End of Life, MND Australia, viewed 3 October 2023, https://www.mndaustralia.org.au/mnd-connect/for-health-professionals-service-providers/end-of-life
- Queensland Brain Institute 2023, Motor Neuron Disease (MND), The University of Queensland, viewed 3 October 2023, https://qbi.uq.edu.au/brain/brain-diseases/motor-neurone-disease
- Queensland Brain Institute 2019, Motor Neuron Disease (MND) Facts and Figures, The University of Queensland, viewed 3 October 2023, https://qbi.uq.edu.au/brain/brain-diseases-and-disorders/motor-neurone-disease/motor-neurone-disease-mnd-facts-and-figures
- Rogers, K 2016, ‘The ‘Ice Bucket Challenge’ Helped Scientists Discover a New Gene Tied to A.L.S.’, The New York Times, 27 July, viewed 3 October 2023, https://www.nytimes.com/2016/07/28/health/the-ice-bucket-challenge-helped-scientists-discover-a-new-gene-tied-to-als.html
 New
New