Hip fractures are potentially catastrophic injuries, particularly in older adults, and are associated with death, disability and loss of independence (Davenport 2021).
Approximately 19,000 people fracture their hip every year in Australia (AIHW 2018). Incidences of hip fractures appear to be increasing as the Australian population ages (Leung et al. 2023).
What is a Hip Fracture?
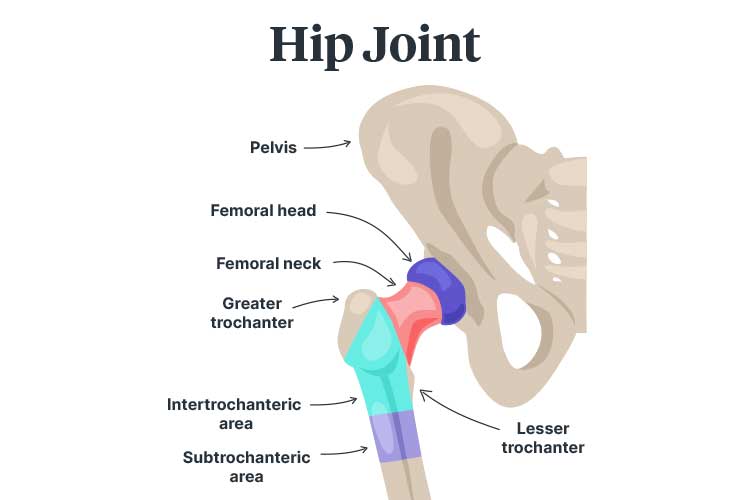
The head of the femur (thigh bone) fits into a socket in the pelvis to form the hip joint (Fischer & Gray 2020).
A hip fracture occurs when the top of the femur cracks or breaks (Fischer & Gray 2020).
Areas where the femur may fracture include:
- The femoral head
- The femoral neck
- The intertrochanteric area (between the greater and lesser trochanters)
- The subtrochanteric area (under the greater and lesser trochanters).
(Fischer & Gray 2020)
Femoral neck fractures are the most common, accounting for about 56% of injuries (AIHW 2018).
Hip fractures are classified according to the extent of displacement:
- Non-displaced fractures occur when the femur cracks without separating
- Minimally displaced fractures occur when the femur shifts along or away from the fracture
- Displaced fractures occur when part of the bone detaches completely.
(Harvard Health Publishing 2020)
Hip fractures are potentially life-threatening, with approximately 8% of injuries resulting in death within 30 days (Leung et al. 2023). Many of those who survive experience permanent impairments to their daily functioning (Mayo Clinic 2022).
Potential consequences of hip fractures and associated immobility include:
- Disability
- Pain
- Loss of independence
- Reduced mobility
- A new need for long-term care
- Pressure injuries
- Deep vein thrombosis, which may lead to pulmonary embolism
- Urinary tract infections
- Pneumonia
- Reduced muscle mass
- Delirium
- Malnutrition.
(ACSQHC 2023; Mayo Clinic 2022)
Hip fractures are most common in older adults over 65 and may indicate poor underlying health (ACSQHC 2023).
Causes of Hip Fractures
Most hip fractures are caused by falls (ACSQHC 2023). In 2015-2016, 93% of new hip fractures were fall-related, with 87% being only minimal trauma falls (AIHW 2018).
Furthermore, hip fractures account for 20% of all fall-related hospital admissions (ACSQHC 2017).
Other potential causes include:
- Severe impact (e.g. a car accident)
- Twisting or tripping
- Standing or walking (in cases of severe bone weakness).
(Mayo Clinic 2022; Fischer & Gray 2020)
Risk Factors for Hip Fractures
- Age, as bone density and muscle mass decrease naturally over time
- Vision and balance issues
- Being female, as the reduction in oestrogen caused by menopause increases bone density loss
- Osteoporosis
- Certain medical conditions that cause bones to weaken, including endocrine disorders and intestinal disorders
- Neurological conditions, which may increase the risk of falling
- Low blood sugar or hypotension, which may increase the risk of falling
- Inadequate calcium and vitamin D intake, which reduces peak bone mass
- Lack of physical activity, which may lead to frailty
- Smoking and alcohol use, which may disrupt bone building and maintenance processes
- Being an Aboriginal or Torres Strait Islander person.
(Mayo Clinic 2022; ACSQHC 2023)
Symptoms of Hip Fractures
- Acute pain in the groin and upper thigh
- Bruising and swelling near the hip
- Difficulty standing
- Difficulty bearing weight on the injured leg
- Difficulty moving, lifting or turning the upper leg or knee
- A noticeable difference in length between legs (the injured leg may look shorter than the other leg)
- The injured leg turning outwards.
(Fischer & Gray 2020; NHS 2023)
Treating Hip Fractures
Most hip fractures require surgery. This should ideally be performed within 48 hours of hospital presentation. Surgery involves using internal fixations to hold the bone together. In some cases, patients require a partial or complete hip replacement (NHS 2023; Mayo Clinic 2022).
Preventing Hip Fractures

Read: Falls Prevention
The main ways to prevent hip fractures are by:
- Preventing falls
- Maintaining bone strength through regular exercise and adequate calcium and vitamin D intake.
(Harvard Health Publishing 2020)
Falls prevention is especially important after an initial hip fracture, as people who have experienced one hip fracture are at increased risk of experiencing another (Sheikh et al. 2019).
Read: Managing Falls Risk After Discharge
Hip Fracture Care Clinical Care Standard
In 2023, the Australia Commission on Safety and Quality in Health Care released the updated Hip Fracture Care Clinical Care Standard. This standard aims to improve assessment and management of hip fractures and reduce the risk of subsequent hip fractures (ACSQHC 2023).
The standard contains seven quality statements:
1. Care at Presentation
Patients who present with a suspected hip fracture should receive prompt assessment and management, including diagnostic imaging, pain relief and assessment of cognition, nutrition and frailty (ACSQHC 2023).
2. Pain Management
Patients with hip fractures should undergo regular pain assessments to ensure they are receiving adequate pain relief. Pain relief may include multimodal analgesia and nerve blocks.
Pain assessments should be performed regularly as part of routine nursing. Additionally, they should be performed:
- Upon presentation
- Within 30 minutes of initial analgesia provision
- Every hour until the patient is settled in the ward.
(ACSQHC 2023)
3. Orthogeriatric Model of Care
Hip fracture treatment should be based on an orthogeriatric model of care, which is defined in the Australian and New Zealand Guideline for Hip Fracture Care. A coordinated interprofessional approach should be used recognise and manage malnutrition, frailty, cognitive impairment and delirium (ACSQHC 2023).
4. Timing of Surgery
Patients should undergo surgery within 36 hours of presentation to hospital (ACSQHC 2023).
5. Mobilisation and Weight-Bearing
Patients should be mobilised starting the day of, or the day after, surgery and then at least once per day (unless there are contraindications). Patients should bear weight on the affected leg depending on their tolerance (ACSQHC 2023).

6. Minimising Risk of Another Fracture
Prior to discharge, patients should be given a falls and bone health assessment and management plan. Prevention strategies may include exercises to improve muscle strength and balance, as well as bone protection medicines if required. Patients may also be referred for secondary fracture prevention (ACSQHC 2023).
7. Transition From Hospital Care
Prior to discharge, patients and their carers should work with clinicians to develop an individualised care plan containing:
- Mobilisation activities
- Post-injury functioning
- Wound care
- Pain management
- Nutrition
- Fracture prevention strategies
- Medicine changes
- New medicines
- Rehabilitation services and equipment.
Upon discharge, a copy of this plan should be forwarded to the patient, their general practitioner and any ongoing clinicians and care providers (ACSQHC 2023).
(ACSQHC 2023)
Test Your Knowledge
Question 1 of 3
True or false: Most hip fractures are caused by falls.
Topics
References
- Australian Commission on Safety and Quality in Health Care 2017, Hip Fracture Care – the Case for Improvement, Australian Government, viewed 19 February 2024, https://www.safetyandquality.gov.au/sites/default/files/migrated/Hip-Fracture-Care-Case-for-Improvement.pdf
- Australian Commission on Safety and Quality in Health Care 2023, Hip Fracture Care Clinical Care Standard, Australian Government, viewed 19 February 2024, https://www.safetyandquality.gov.au/publications-and-resources/resource-library/hip-fracture-clinical-care-standard-2023
- Australian Institute of Health and Welfare 2018, Hip Fracture Incidence and Hospitalisations in Australia 2015–16, Australian Government, viewed 19 February 2024, https://www.aihw.gov.au/reports/injury/hip-fracture-incidence-in-australia-2015-16/contents/summary
- Davenport, M 2021, Hip Fracture in the ED, Medscape, viewed 19 February 2024, https://emedicine.medscape.com/article/825363-overview
- Fischer, SJ & Gray, JL 2020, Hip Fractures, OrthoInfo, viewed 19 February 2024, https://orthoinfo.aaos.org/en/diseases--conditions/hip-fractures/
- Harvard Health Publishing 2020, Hip Fracture, Harvard College, viewed 19 February 2024, https://www.health.harvard.edu/a_to_z/hip-fracture-a-to-z
- Leung, MTY et al. 2023, ‘Hip Fracture Incidence and Post-Fracture Mortality in Victoria, Australia: A State-Wide Cohort Study’, Arch Osteoporos., vol. 18, no. 1, viewed 19 February 2024, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10148778/
- Mayo Clinic 2022, Hip Fracture, Mayo Clinic, viewed 19 February 2024, https://www.mayoclinic.org/diseases-conditions/hip-fracture/symptoms-causes/syc-20373468
- National Health Service 2023, Broken Hip, NHS, viewed 20 February 2024, https://www.nhs.uk/conditions/broken-hip/
- Sheikh, H Q, Hossain, F S, Khan, S, Usman, M, Kapoor, H & Aqil, A 2019, ‘Short-Term Risk Factors for a Second Hip Fracture in a UK Population’, European Journal of Orthopaedic Surgery & Traumatology, vol. 29, no. 5, viewed 20 February 2024, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6570666/
Additional Resources
- Hip Fracture Care Clinical Care Standard | ACSQHC
- Australian and New Zealand Guideline for Hip Fracture Care | ANZHFR
- An Overview of Osteoporosis | Ausmed Article
- Falls Prevention | Ausmed Article
- Managing Falls Risk After Discharge | Ausmed Article
- Minimising Falls Risk in the Home | Ausmed Article
- Falls Prevention at the Bedside | Ausmed Course
- Falls: Psychosocial Care | Ausmed Course
- Identifying Falls Risk | Ausmed Course
 New
New