Time management involves consciously planning and organising how you are going to allocate your time between activities (Mind Tools n.d.).
When used effectively, time management is a useful skill that allows you to get more done in less time, even under time pressure (Mind Tools n.d.).
For healthcare professionals, who have tasks constantly competing for their attention and need to juggle a variety of stressors on a daily basis, time management is particularly essential.
What are the Benefits of Good Time Management?
Effective time management has several benefits, including:
- Increased productivity and efficiency
- Reduced stress and burnout
- Improved patient care
- Increased personal satisfaction
- Increased opportunities for career advancement.
(Mind Tools n.d.; MIPS 2023)
Poor time management, on the other hand, can result in undesirable outcomes like increased patient waiting times, unnecessary stress, reduced enjoyment at work and less time for other priorities like family, sleep and exercise (MIPS 2023).
With this in mind, what techniques can healthcare professionals use to manage their time more effectively?
Prioritise
It’s important to ‘prioritise prioritising’ (Bibic, as cited in Rimmer 2019).
At the start of your shift, you will normally have a list of tasks that you need to do, ranked by which is the most important.
When you prioritise, you systematically pick the task or patient that is the most important and address them first. This has to be a conscious decision. Patients with critical lab work or abnormal vital signs must take priority over routine tasks, for example.
This may seem like common sense, but it can get tricky in a high-stress situation. Just remember that patient safety is always your best bet when prioritising tasks.
If the patient’s safety is not in question, then you have to prioritise via other criteria, such as patient needs, the potential for patient safety, or the time sensitivity of a task. Even when there is no critical issue at stake, knowing which tasks need doing first helps you navigate the sheer volume that you have to face when you start your shift.
Helpful questions to ask yourself include:
- Which tasks do you think should be done first?
- Which tasks are the most urgent?
- Which tasks can only be carried out after performing another task first?
- What are the consequences, if any, of not performing certain tasks immediately?
- Which tasks are most important to your patients?
(Dragon 2019; Woogara 2012)
It might be helpful to roughly estimate how long each task should take, which will prevent you from spending too much time doing one thing (Dragon 2019).
One tool that can help you prioritise your work is a decision matrix.
A decision matrix helps you to sort your tasks into four categories, allowing you to determine what needs to be done first. It can be used to prioritise both short and long-term goals (MIPS 2023).
See the example below:
| Urgent | Less urgent | |
|---|---|---|
| Important | Attending to a deteriorating patient | Changing wound dressings |
| Less important | Returning a call from patient’s relative | Checking emails |
(Adapted from MIPS 2023)
Tasks that are urgent and important should be prioritised first, while tasks that are less urgent and less important can wait until the more important and urgent tasks have been completed.
Other strategies include:
- Giving each of your tasks a number between 1 and 10 to indicate urgency
- Sorting your tasks into categories (e.g. ‘discharges’), then determining which categories need to be prioritised
- Using the 80/20 rule (i.e. 20% of your tasks should take 80% of your time, and the other 80% of your tasks should take the remaining 20% of your time).
(Woogara 2012; MIPS 2023)
Tasks that aren’t on your to-do list, for example, having long chats with colleagues, should be avoided (Woogara 2012).
Arrive at Work Early
Arriving early will give you extra time to read through important documents (e.g. reports and handover sheets), organise your tasks for the day and get a sense of the vibe in your workplace (Dragon 2019; Woogara 2012).
Even arriving 5 or 10 minutes early can be beneficial and help you to settle in before starting your shift (Dragon 2019).
Take Notes
Notes can be in whatever form you like, for example, to-do lists, grids or tick boxes next to your handover notes. You might want to write down the care that each patient requires for the day and when it needs to be delivered, patients’ ambulatory and dietary requirements, and other specific patient needs. This will help you remember what needs to be done and when (Dragon 2019; Woogara 2012).
Use a Time Management Sheet
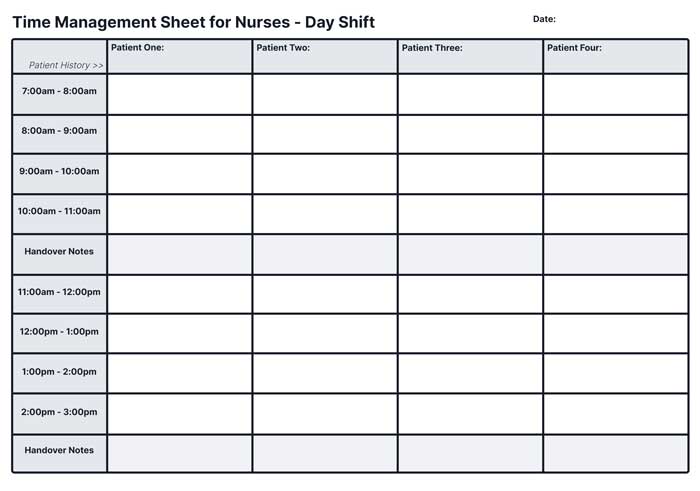
One of the hallmark ways to manage your time is to work to a schedule, and many do this by using a worksheet to mark down important information about their patients.
A time management sheet may have spaces for lab work, new orders, medication times and other important information that you need to remember throughout the day. Ask more experienced colleagues for blank copies of their sheets and use them for a few days. Once you have an idea of what works and doesn’t work for you, sit down with a word processor or spreadsheet program and make a flowchart of your own that organises all the important information you need on each patient for the shift.
It takes a trial and error process to get a sheet that works right for you, but once you find the right combination, your days will run a lot smoother.
Be Flexible
Be prepared to reassess your to-do list as your priorities change throughout the day (Woogara 2012).
It’s important to leave time for unexpected events, just in case you suddenly need to perform extra tasks. Be prepared for the unpredictable, such as:
- Sudden patient deterioration or death
- Sudden admissions
- Staff becoming unwell and going home
- Relatives asking questions.
(Dragon 2019)
Despite your best-laid plans, you will meet many interruptions.
Having a plan to go back to after you’ve finished dealing with an interruption is essential. The trick is to not get so attached to a time management plan that any deviation makes you shrivel up into a ball.
You need to deal with the interruption - a code blue, a fall, a doctor’s call - and then calmly go back to your other duties, reprioritise what needs to be done and start from the beginning again.
Be Organised

Being tidy and putting things back where they came from will save you time looking for them. Furthermore, being organised reduces the risk of hazards (e.g. clutter) and will help you feel more ‘in control’ (Dragon 2019).
It may also be helpful to anticipate the equipment you’ll need in the future and gather it all at once instead of wasting time making multiple trips (Dragon 2019).
Delegate
Delegation involves directing a coworker to perform a certain task under appropriate supervision (Barrow & Sharma 2023).
When used appropriately, delegation saves time, increases productivity and allows other healthcare professionals to further develop their skills (Rivier University 2017).
Consider the following Five Rights of Nursing Delegation before proceeding:
- Right Task: Ensure the task is appropriate for the delegatee and falls within their scope. You must be confident that the delegate can perform the task safely and correctly.
- Right Circumstance: Make sure you only delegate tasks at an appropriate time - for example, avoid doing so if the patient is unstable or in a critical condition.
- Right Person: Only delegate a task to someone who has demonstrated skills and knowledge in that particular area.
- Right Directions/Communication: Communicate clearly and precisely with the delegate. Outline your expectations and answer any questions they may have.
- Right Supervision/Evaluation: As the delegator, the outcome of the task is still your responsibility. You need to be available to supervise, make corrections and provide feedback to the delegate.
(Rivier University 2017)
Say ‘No’
Inevitably, some tasks will need to wait. You’re allowed to say ‘no’ to requests for help from coworkers and patients if they’re not urgent (Dragon 2019; Woogara 2012).
Setting boundaries is important in preventing burnout and, consequently, poorer patient outcomes (Rimmer 2019).
Be Efficient
Effective management doesn’t mean taking shortcuts or guessing - remember that the consequences of making mistakes may be worse than taking extra time to perform a task. Always take the time to double-check if you are unsure of something (Dragon 2019).
Listen

Don’t assume that you and the patient are on the same page. Instead of assuming their priorities, ask them. This will prevent you from spending time on unnecessary tasks (Woogara 2012).
Exercise Self-Care
‘Self-care is not a luxury, it’s a responsibility.’ (Smith, as cited in Rimmer 2019)
Burnout among healthcare professionals has been found to be associated with poorer patient care and reduced patient satisfaction (Panagioti et al. 2018).
Therefore, it’s in the best interests of yourself, as well as your patients, to exercise self-care when needed. Examples include:
- Taking a quick break to collect your thoughts if you’re feeling overwhelmed
- Remembering to go to the toilet and take meal breaks, even if it’s a busy shift
- Being kind to yourself
- Maintaining a good work-life balance
- Having fun where appropriate
- Getting outside when possible
- Making plans outside of work
- Do things that bring you joy and personal satisfaction.
(Dragon 2019; Nelson 2021; Rimmer 2019)
Self-Care Tools for Healthcare Professionals and Staff
You may also want to try specific techniques, such as meditation, in order to improve your self-care.
A variety of evidence-based mindfulness and self-care exercises that have been designed specifically with healthcare workers in mind can be accessed through the Ausmed app’s Mindfulness Corner.
Conclusion
Getting tasks done is important, but sometimes, you won’t be able to finish everything on your to-do list. Time management is a skill that requires practice in order to be mastered, so instead of being hard on yourself, reflect and find areas for improvement (Dragon 2019).
Finally, remember that some things are outside of your control, even if you prioritise as best you can (Dragon 2019).
Test Your Knowledge
Question 1 of 3
Finish the sentence. According to the 80/20 rule …
Topics
References
- Barrow, JM & Sharma, S 2020, ‘Five Rights of Nursing Delegation’, StatPearls, viewed 22 January 2024, https://www.ncbi.nlm.nih.gov/books/NBK519519/
- Dragon, N 2019, ‘10 Time Management Tips for Nurses and Midwives’, Australian Nursing and Midwifery Journal, 1 August, viewed 22 January 2024, https://anmj.org.au/10-time-management-tips/
- Medical Indemnity Protection Society 2023, Smart Time Management For Healthcare Practitioners, MIPS, viewed 22 January 2024, https://support.mips.com.au/home/smart-time-management-for-healthcare-practitioners
- Mind Tools n.d., What Is Time Management?, Mind Tools, viewed 22 January 2024, https://www.mindtools.com/pages/article/newHTE_00.htm
- Nelson, L 2021, ‘Top Time Management Skills for Nurses’, Nurse.org, 20 January, viewed 22 January 2024, https://nurse.org/articles/effective-time-management-skills-for-nurses/
- Panagioti, M et al. 2018, ‘Association Between Physician Burnout and Patient Safety, Professionalism, and Patient Satisfaction: A Systematic Review and Meta-Analysis’, JAMA Intern Med., vol. 178, no. 10, viewed 22 January 2024, https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2698144
- Rimmer, A 2019, ‘How Do I Improve My Time Management Skills?’, BMJ, viewed 22 January 2024, https://www.bmj.com/content/366/bmj.l5322
- Rivier University 2017, Tips to Master Delegation in Nursing, Rivier University, viewed 22 January 2024, https://www.rivier.edu/academics/blog-posts/tips-to-master-delegation-in-nursing/
- Woogara, N 2012, ‘10 Ways to Effectively Manage Your Time on the Ward’, Nursing Times, 30 March, viewed 22 January 2024, https://www.nursingtimes.net/archive/10-ways-to-effectively-manage-your-time-on-the-ward-30-03-2012/
 New
New 
