Electrolyte imbalances can occur due to hundreds of factors, none of which line up in neat, tidy queues.
Look at a few of the most common examples:
- Patients experiencing congestive heart failure often end up with rebound hospitalisations due to abnormal sodium and potassium levels.
- A grandmother with diabetes or hypertension may eventually find herself on the business end of a calcium or magnesium imbalance.
- The toddler with explosive diarrhoea and the elite Australian athlete, otherwise wildly unalike, both routinely find themselves on the business end of electrolyte imbalances.
A proper understanding of these imbalances is essential for current management and future prevention.
Facts and Figures
Electrolyte imbalances occur across many different diagnostic categories.
In Australia, harsh summer environmental exposure, with resulting dehydration, is just one example of a potential root cause (Roumelioti et al. 2018); sadly, more Australians are killed from the ill effects of heatwaves than all other natural hazards (Healthdirect 2023).
This is just one potential cause, however. There are hundreds of other root causes for fluid and electrolyte imbalances, including:
- In children: A leading cause of dehydration and electrolyte imbalance is acute gastroenteritis, an illness that can be effectively treated with oral rehydration.
- In older people: One of the primary reasons older populations are at an elevated risk of dehydration and electrolyte imbalance is a diminished thirst response.
- In athletes: Electrolyte imbalances during exercise come from multiple sources. Strangely, the muscles doing work do not lose water content during exercise; rather, they dehydrate during the immediate post-exercise recovery period, presumably in an effort to restore plasma volume and stabilise the cardiovascular system.
(Santillanes & Rose 2018; Picetti et al. 2017; Mora-Rodríguez et al. 2014; AIS 2021)

What is an Electrolyte Imbalance?
Put simply, electrolytes are naturally occurring minerals with an electric charge.
They exist in the human body and are also present in food and fluids we ingest every day.
Potassium, magnesium and sodium are several commonly known electrolytes, but they are not alone; calcium and phosphate also play critical roles. These electrolytes serve crucial functions in the body such as keeping water in balance, regulating the body’s base pH levels and moving nutrients and waste to and from cells (MedlinePlus 2024).
Symptoms of Electrolyte Imbalance
Electrolyte imbalance can be a marker of many common diseases and illnesses.
Assessing a patient for electrolyte imbalance can give practitioners insight into the body's homeostasis and can serve as a marker or proxy for the presence of other illnesses.
Practitioners can assess for electrolyte imbalance using physical examination, ECGs, serum electrolyte levels and pathologic signs.
Certain symptoms can even point to a specific electrolyte that is out of balance in a patient. For example, confusion is a common symptom of hypocalcaemia (Lewis III 2023).
By using the aforementioned examination techniques, practitioners can pinpoint which electrolytes are out of balance and thus craft a more effective treatment plan for the patient.
What Causes an Electrolyte Imbalance?
Dehydration does not occur at some standardised setpoint; it is caused by consuming too little fluid for the body's present needs.
This can happen through either decreased consumption or outside factors that cause the body to require more water than normal.
Whenever the body is overhydrated or underhydrated - or when the body’s filtration systems do not operate normally - electrolytes no longer function as they should.
Abnormal electrolyte levels can occur any time the body’s fluid levels fluctuate outside of norms, such as after serious burns, vomiting, diarrhoea or excessive sweating.
Infrequently, overhydration can also result in serious repercussions. Certain medicines and dysfunctions of the liver and kidneys can also throw the body’s electrolytes out of normal range.
Risk Factors for Electrolyte Imbalance
While anyone can develop an electrolyte disorder, the older population is at increased risk. Some factors that can increase the risk of an electrolyte imbalance in older populations include:
- Reduced kidney function with age
- Inadequate food and fluid intake due to factors such as disability, lack of appetite or thirst, or reduced access to foods and drinks
- The use of diuretics (which promote fluid excretion by the kidneys).
(Tinsley & Berry 2023)
Within these risk factors, there is an increased risk for those who use certain combinations of diuretics and for those with diabetes. Patients who use both thiazides and benzodiazepines are associated with higher rates of hyponatremia, which, in turn, is associated with a higher mortality risk (Liamis 2013).
The use of angiotensin-converting enzyme inhibitors (ACE inhibitors), potassium and calcium supplements, and certain hormones, which are classified as potassium-sparing, can also lead to imbalances.
Other factors that can increase the risk of an electrolyte disorder include, but are not limited to:
- Burns
- Significant trauma (such as broken bones)
- Congestive heart failure
- Substance use disorder
- Kidney disorders
- Diarrhoea or vomiting
- Heat exhaustion
- Eating disorders (such as anorexia or bulimia)
- Thyroid, parathyroid, and adrenal gland disorders (such as Addison’s disease).
(Cleveland Clinic 2022; Bernstein & Holland 2022)
Diagnosing an Electrolyte Imbalance
There are several types of tests that can be used to diagnose electrolyte imbalance. Each type of test has its own pros and cons for detecting various types of imbalances. Here are just a few of the ways practitioners test for electrolyte dysfunction:
- The anion gap blood test analyses the level of acid in the blood. This can indicate an electrolyte imbalance, as electrolytes balance the pH of the blood.
- Carbon dioxide blood tests measure CO2 levels in the blood. CO2 in the blood is often in the form of an electrolyte called bicarbonate.
- Chloride tests measure the levels of chloride, another electrolyte, in the blood.
- Sodium blood tests analyse sodium levels in the blood, another common portion of an electrolyte blood panel.
(MedlinePlus 2024)
Treating Electrolyte Imbalances

Individuals who experience serious symptoms, tachycardia, mental confusion, sunken eyes, reduced elasticity of the skin, and/or a loss of consciousness need immediate medical attention.
People who dehydrate through exercise or activity can typically turn to sports drinks for electrolyte restoration. Australia’s AIS Sports Supplement Framework, an initiative of AIS Sports Nutrition, has published an excellent guide to the use of such sports drinks.
Between these two extremes is a vast middle ground with some patients requiring rapid - though not emergency - medical assistance, and some patients self-correcting without ever knowing anything more than that they 'felt a bit off'.
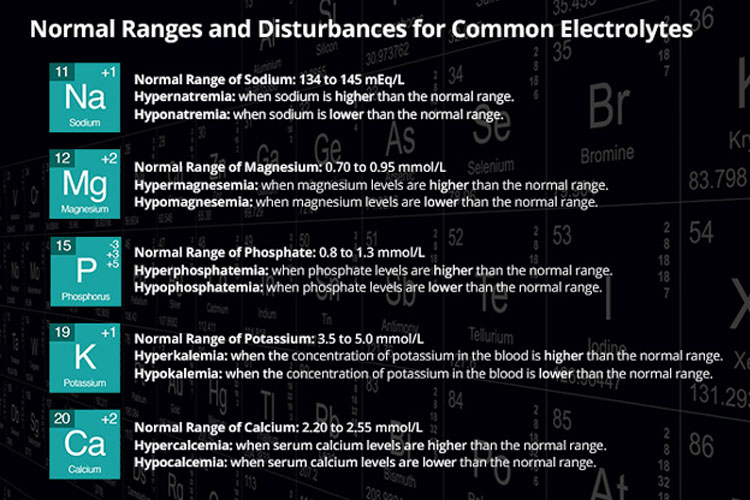
Normal Ranges and Disturbances of Common Electrolytes
Although many trace elements keep the body healthy, several important electrolytes can severely affect patients when they are either too high (hyper...) or too low (hypo...).
Understanding what each electrolyte does and what happens when there isn't enough of one or too much of another is essential knowledge for nurses and can help guide electrolyte therapy.
Sodium
Sodium, or Na, is one of the most important electrolytes in the body and is responsible for a number of important functions, mostly related to fluid and water regulation. The normal accepted range for sodium is 135 to 145 mEq/L (NKF 2024).
Hyponatraemia is defined as serum sodium below 135 mEq/L. A common cause is water retention due to cardiac, renal, or hepatic failure. Other causes of hyponatraemia include some medicines, psychogenic polydipsia (excessive water intake), syndrome of inappropriate antidiuretic hormone secretion (SIADH), and chronic or severe vomiting and diarrhoea (NKF 2024).
Common symptoms of hyponatraemia include confusion, agitation, nausea and vomiting, muscle weakness, spasms and cramps (NKF 2024).
Hypernatraemia is defined as a serum sodium greater than 145 mEq/L (ACI 2024a).
Causes of hypernatraemia are simply anything that leads to excessive water loss or salt gain. For example, water depletion or dehydration may be caused by vomiting and diarrhoea.
Excessive ingestion of sodium is rare, but the administration of infusions containing sodium such as sodium chloride or sodium bicarbonate may lead to hypernatraemia.
Clinical features of hypernatraemia may include fever, irritability, lethargy and confusion (ACI 2024a).
Potassium
Potassium, or K, is responsible for the functioning of excitable tissues such as skeletal and cardiac muscle and nerves. The normal range for potassium in adults is 3.5 to 5.0 mmol/L (Colbert 2024).
Hypokalaemia is defined as serum potassium less than 3.5 mmol/L. Low serum potassium may be caused by decreased oral intake, increased renal or gastrointestinal loss of potassium, or a shift of potassium within the body's fluid compartments (from outside the cell where it should be, to inside the cell) (Lederer 2023).
Common clinical features of hypokalaemia range from muscle weakness and ileus (lack of peristalsis) to serious cardiac arrhythmias (Lederer 2023).
Hyperkalaemia, a serum potassium of greater than 5.0 to 5.5 mmol/L (typically), may be caused by excessive intake, tissue damage from burns or trauma, medicines such as potassium-sparing diuretics or renal failure (Simon et al. 2023).
Most cases of hyperkalaemia are asymptomatic. Some patients may experience muscle weakness, fatigue, heart palpitations or loss of consciousness. ECG changes may include peaked T waves and flattened P waves (Simon et al. 2023).
Magnesium

Magnesium, or Mg, is another element that strongly affects muscle contractions. The normal plasma range for magnesium in adults is 0.70 to 1.10 mmol/L (Pathology Tests Explained 2023a).
Hypomagnesaemia, or a decreased plasma magnesium level, may be caused by decreased intake or increased loss of magnesium. Clinical signs can include confusion, irritability, delirium, muscle tremors and ventricular arrhythmias (Gragossian et al. 2023).
Hypermagnesaemia occurs when the magnesium level in the blood is above the normal range. Fortunately, it is uncommon. Symptoms include poor reflexes, hypotension, respiratory depression and cardiac arrest. It is usually caused by the excessive administration of magnesium and lithium therapy, often in the presence of renal failure (ACI 2024b).
Calcium
Calcium, or Ca, is an important element in the body. It helps to control nerve impulses and muscle contractions and plays a role in clotting. When normal, the serum calcium range should be between 2.10 and 2.60 mmol/L (Pathology Tests Explained 2023b).
Hypocalcaemia, the presence of low serum calcium levels in the blood, is relatively rare because the bones always act as a reservoir for this electrolyte. However, parathyroid disease, vitamin D deficiency, septic shock, and acute pancreatitis can cause this problem. Some symptoms include tetany (involuntary muscle contraction), mental state changes and seizures (Goyal et al. 2023).
Hypercalcaemia, elevated levels of calcium in the blood, again arises from parathyroid problems and vitamin D issues. Signs of this form of electrolyte imbalance include nausea and vomiting, polyuria, muscular weakness and mental disturbance (Mayo Clinic 2024).
Phosphate
Phosphate, or P, is an electrolyte used in several functions throughout the body. Although a phosphate imbalance isn't as well known as some of the other imbalances, it can still cause problems with your patient's condition. The normal range of phosphate in the plasma is generally between 0.8 to 1.5 mmol/L (ACI 2024c). The signs and symptoms of either abnormal reading are usually subtle.
Hypophosphataemia is where levels of phosphate in the blood are below the normal range. Most cases are asymptomatic, but the most common sign is muscle weakness. Severe cases may present with symptoms such as mental status changes, seizures and cardiac failure (Sharma et al. 2024).
Hypophosphataemia may be caused by vitamin D deficiency, hyperparathyroidism or alcohol abuse. It may also be present in addition to other electrolyte disturbances in re-feeding syndrome, which is associated with the commencement of total parental nutrition (TPN) (Sharma et al. 2024).
Hyperphosphataemia occurs when levels of phosphate in the blood are above the normal range. It can be caused by kidney disease, parathyroid issues and metabolic or respiratory acidosis. Symptoms are usually not present, and they are related to hypocalcaemia. Renal patients can experience hardened calcium deposits when this condition goes untreated (Goyal & Jialal 2023).
Complications of Electrolyte Imbalances
Some examples of complications that can be caused by electrolyte imbalances include:
- Epileptic encephalopathies from hypomagnesaemia and dysnatraemias
- Cardiac arrhythmias from hypocalcaemia and dyskalaemias
- Muscle weakness, lethargy, and fatigue from potassium, calcium and magnesium imbalances.
(Shrimanker & Bhattarai 2023)
Conclusion
Many electrolyte imbalances self-correct without any ill effects. A simple drink of water can correct others.
However, electrolyte imbalances can be much more than just a nuisance - they may cause severe complications when left untreated. It is important for practitioners to correctly test for and diagnose electrolyte imbalances in order to treat them in an appropriate and timely fashion.
Test Your Knowledge
Question 1 of 3
Which population is at an increased risk for dehydration and electrolyte imbalances due to a diminished thirst response?
Topics
References
- Agency for Clinical Innovation 2024b, Magnesium - Hypermagnesemia, New South Wales Government, viewed 13 August 2024, https://aci.health.nsw.gov.au/networks/eci/clinical/clinical-tools/electrolytes/magnesium-hypermagnesemia
- Agency for Clinical Innovation 2024c, Phosphate - Hypophosphataemia, New South Wales Government, viewed 13 August 2024, https://aci.health.nsw.gov.au/networks/eci/clinical/clinical-tools/electrolytes/phosphate-hypophosphataemia
- Agency for Clinical Innovation 2024a, Sodium - Hypernatraemia, New South Wales Government, viewed 13 August 2024, https://aci.health.nsw.gov.au/networks/eci/clinical/clinical-tools/electrolytes/sodium-hypernatraemia
- Australian Institute of Sport 2021, Sports Drinks (Carbohydrate-Electrolyte Drinks), AIS, viewed 13 August 2024, https://www.ais.gov.au/__data/assets/pdf_file/0009/998802/36194_Sport-supplement-fact-sheets-Sports-drinks-v4.pdf
- Bernstein, A & Holland, K 2022, ‘All About Electrolyte Imbalance’, Healthline, 15 December, viewed 13 August 2024, https://www.healthline.com/health/electrolyte-disorders
- Cleveland Clinic 2022, Electrolyte Imbalance, Cleveland Clinic, viewed 13 August 2024, https://my.clevelandclinic.org/health/symptoms/24019-electrolyte-imbalance
- Colbert, GB 2024, Potassium, Medscape, viewed 13 August 2024, https://emedicine.medscape.com/article/2054364-overview
- Goyal, A, Anastasopoulou, C, Ngu, M & Singh, S 2023, ‘Hypocalcemia’, StatPearls, viewed 13 August 2024, https://www.ncbi.nlm.nih.gov/books/NBK430912/
- Goyal, R & Jialal, I 2023, ‘Hyperphosphatemia’, StatPearls, viewed 13 August 2024, https://www.ncbi.nlm.nih.gov/books/NBK551586/
- Gragossian, A, Bashir, K, Bhutta, BS & Friede R 2023, ‘Hypomagnesemia’, StatPearls, viewed 13 August 2024, https://www.ncbi.nlm.nih.gov/books/NBK500003/
- Healthdirect 2023, Hot Weather Risks and Staying Cool, Australian Government, viewed 13 August 2024, https://www.healthdirect.gov.au/hot-weather-risks-and-staying-cool
- Lederer, E 2023, Hypokalemia, Medscape, viewed 13 August 2024, https://emedicine.medscape.com/article/242008-overview
- Lewis, JL III 2023, Hypocalcemia (Low Level of Calcium in the Blood), MSD Manual, viewed 13 August 2024, https://www.msdmanuals.com/en-au/home/hormonal-and-metabolic-disorders/electrolyte-balance/hypocalcemia-low-level-of-calcium-in-the-blood
- Liamis, G, Rodenburg, EM, Hofman, A et al. 2013, 'Electrolyte Disorders in Community Subjects: Prevalence and Risk Factors', The American Journal of Medicine, vol. 126, no. 3, pp. 256-63, viewed 13 August 2024, https://www.amjmed.com/article/S0002-9343(12)00789-9/fulltext
- Mayo Clinic 2024, Hypercalcemia, Mayo Clinic, viewed 13 August 2024, https://www.mayoclinic.org/diseases-conditions/hypercalcemia/symptoms-causes/syc-20355523
- Mora‐Rodríguez, R, Fernández‐Elías, VE, Hamouti, N & Ortega, JF 2015, 'Skeletal Muscle Water and Electrolytes Following Prolonged Dehydrating Exercise', Scandinavian Journal of Medicine & Science in Sports, vol. 25, no. 3, e. 274-82, viewed 13 August 2024, https://onlinelibrary.wiley.com/doi/abs/10.1111/sms.12316
- MedlinePlus 2024, Fluid and Electrolyte Balance, U.S. Department of Health and Human Services, viewed 13 August 2024, https://medlineplus.gov/fluidandelectrolytebalance.html
- National Kidney Foundation 2024, Hyponatremia (Low Sodium Level in the Blood), NKF, viewed 13 August 2024, https://www.kidney.org/atoz/content/hyponatremia
- Pathology Tests Explained 2023b, Calcium, Pathology Tests Explained, viewed 13 August 2024, https://pathologytestsexplained.org.au/ptests.php?q=Calcium
- Pathology Tests Explained 2023a, Magnesium, Pathology Tests Explained, viewed 13 August 2024, https://pathologytestsexplained.org.au/ptests-pro.php?q=Magnesium
- Picetti, D, Foster, S, Pangle, AK et al. 2017, ‘Hydration Health Literacy in the Elderly’, Nutr Healthy Aging., vol. 4 no. 3, viewed 13 August 2024, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5734130/
- Roumelioti, ME, Glew, RH, Khitan, ZJ et al. 2018, 'Fluid Balance Concepts in Medicine: Principles and Practice', World Journal of Nephrology, vol. 7, no. 1, pp. 1, viewed 13 August 2024, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5760509/
- Santillanes, G & Rose, E 2018, 'Evaluation and Management of Dehydration in Children', Emergency Medicine Clinics, vol. 36, no. 2, pp. 259-73, viewed 13 August 2024, https://www.sciencedirect.com/science/article/pii/S0733862717301396?via%3Dihub
- Sharma, S, Hashmi, MF, Kaur, J & Castro D 2024, ‘Hypophosphatemia’, StatPearls, viewed 13 August 2024, https://www.ncbi.nlm.nih.gov/books/NBK493172/
- Shrimanker, I & Bhattarai, S 2023, ‘Electrolytes’, StatPearls, viewed 13 August 2024, https://www.ncbi.nlm.nih.gov/books/NBK541123/
- Simon, LV, Hashmi, MF & Farrell, MW 2023, ‘Hyperkalemia’, StatPearls, viewed 13 August 2024, https://www.ncbi.nlm.nih.gov/books/NBK470284/
- Tinsley, G & Berry, J 2023, ‘Electrolyte Imbalance Symptoms, What Causes it, and How to Treat it’, MedicalNewsToday, 20 December, viewed 13 August 2024, https://www.medicalnewstoday.com/articles/electrolyte-imbalance
 New
New