Untreated, glaucoma can cause blindness (CERA 2020).
Despite this, among the estimated 300,000 Australians living with glaucoma, only half are aware that they have the disease (CERA 2020).
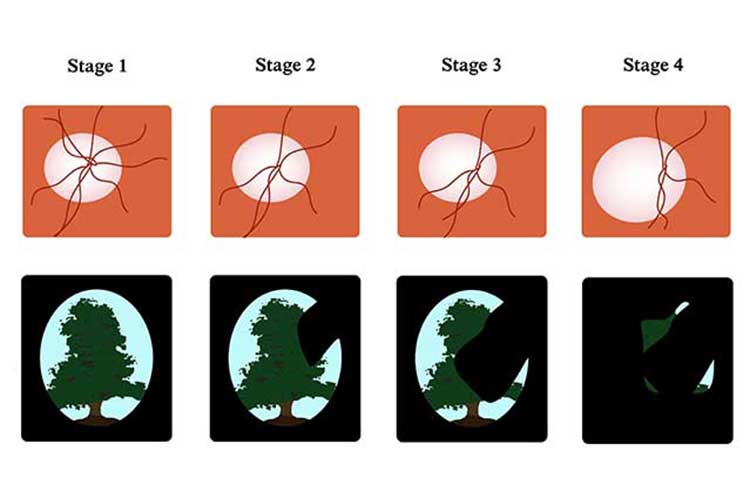
This may be because the onset of glaucoma can be a gradual one. So much so that a significant amount of side vision will be lost before the individual has even noticed they have a condition (Glaucoma Australia 2017a).
What is Glaucoma?
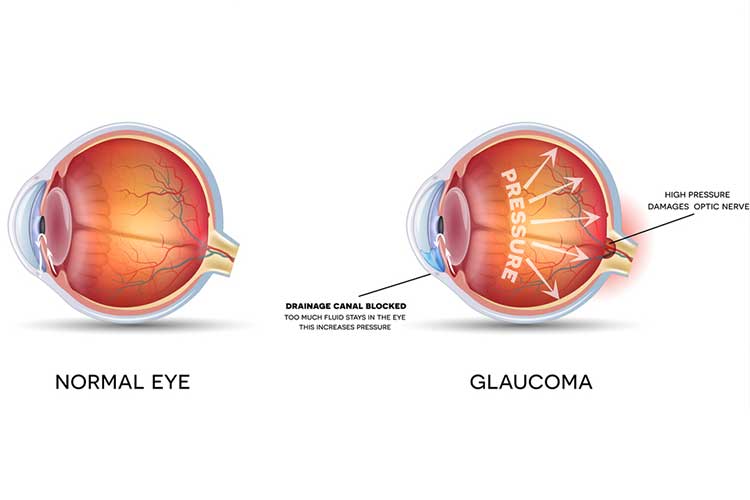
Glaucoma is the name given to a range of conditions that lead to optic nerve damage. The optic nerve transmits signals from the eye to the brain to create the image we see (Vision Eye Institute 2022).
If a considerable number of nerve fibres are affected, the peripheral field of vision is lost - this loss slowly creeps toward the central vision. Currently, glaucoma cannot be reversed (Vision Eye Institute 2022).
Types of Glaucoma
Glaucomas can typically be separated into two subgroups:
- Open-angle glaucoma (where the drain of the eye is fully open)
- Closed-angle glaucoma (where the drain of the eye is partially or fully blocked).
(Glaucoma Australia 2017b)
Furthermore, glaucomas can be either primary (unknown cause) or secondary (caused by another condition) in nature (Glaucoma Australia 2020).
Common types of primary glaucoma include:
Primary Open-Angle Glaucoma
Primary open-angle glaucoma (POAG) causes a patient to lose their peripheral vision due to damage to the optic nerve. Insufficient fluid drainage from the eye is responsible for pressure and nerve damage (Glaucoma Australia 2017b).
This type of glaucoma typically does not cause pain and is, therefore, difficult to detect. As with other types of glaucoma, the early signs may be very subtle (Glaucoma Australia 2017b).
POAG is the most common type of glaucoma - it is responsible for around 90% of reported glaucoma cases in Australia (Glaucoma Australia 2017a).
Normal Tension Glaucoma
Normal tension glaucoma is the term given to cases in which the patient has ‘normal’ eye pressure and therefore, other reasons must be considered in determining changes in nerve pressure and visual field loss (Glaucoma Australia 2017b).
Normal tension glaucoma accounts for roughly one-third of glaucoma cases in Australia (Glaucoma Australia 2017b).
Primary Angle-Closure (PAC) and Primary Angle-Closure Glaucoma (PACG)
A primary angle-closure (PAC) is a result of an inherited narrowness of the eye's drainage angle. Aqueous fluid must drain through the angle between the trabecular meshwork and the iris, and in this condition, it is unable to (Glaucoma Australia 2017b).
The term primary angle-closure glaucoma (PACG) refers to optic nerve damage caused by a PAC (Glaucoma Australia 2017b).
PAC and PACG are more common in long-sighted people, older adults, females, and/or people of Asian background (Glaucoma Australia 2017b).
Acute Angle-Closure Glaucoma
People with PAC and/or PACG may be prone to experiencing an acute angle-closure glaucoma attack. This is a medical emergency requiring urgent intervention (Glaucoma Australia 2017b).
Symptoms of an acute attack may include blurry vision, coloured rings around lights, severe eye pain, redness, nausea and vomiting (Glaucoma Australia 2017b).
Childhood Glaucoma
An abnormal drainage system is responsible for childhood glaucoma. It can be detected by noticing that children are particularly sensitive to light and have excessively cloudy and watery eyes (Glaucoma Australia 2017b).
Childhood glaucoma is rare and devastating when it does occur. Cases tend to vary in severity. (Glaucoma Australia 2017b).
Symptoms of Glaucoma
Symptoms most often associated with glaucoma include:
- Painless but blurred vision
- Loss of peripheral vision
- Trouble adjusting to low light.
(Vision Australia 2017)
Risk Factors for Glaucoma
Those with a family history of glaucoma are at the greatest risk of developing this condition. In fact, having a first-degree relative with glaucoma increases the risk of developing glaucoma ten-fold (CERA 2020).
Other main predictors include:
- Age (over 40-50)
- High intraocular (eye) pressure
- Myopia (short-sightedness) or hyperopia (long-sightedness)
- Diabetes mellitus
- Migraines
- History of eye surgery or injury
- Prolonged use of steroid medicines
- Hyper or hypotension.
(Vision Australia 2017; Healthdirect 2022)
Those in high-risk categories should have their eyes checked regularly (Vision Australia 2017).
Diagnosing Glaucoma

If a doctor or optometrist suspects a person may have glaucoma, they may be referred to an ophthalmologist for further investigation and analysis. A range of eye tests will then be taken in order to confirm the diagnosis (Vision Eye Institute 2024).
Treating Glaucoma
While damaged nerve cells caused by glaucoma are irreversible, there is treatment available to prevent or delay further damage, primarily by reducing the pressure in the eye.
Typically, this involves:
- Eye drops or medicine
- Laser surgery or other surgery to open or create a new drainage channel.
(Healthdirect 2022)
Preventing Glaucoma
Regular eye tests are the most effective way to prevent glaucoma - early diagnosis and treatment are essential (CERA 2020).
Further Information
To gain a better understanding of glaucoma, Glaucoma Australia has curated a list of several stories from the perspectives of people living with the condition: https://www.glaucoma.org.au/about-glaucoma/glaucoma-stories/
Test Your Knowledge
Question 1 of 3
What increases a person’s risk of developing glaucoma ten-fold?
Topics
References
- Centre for Eye Research Australia 2020, Glaucoma, CERA, viewed 3 July 2024, https://www.cera.org.au/conditions/glaucoma/
- Glaucoma Australia 2017b, Types of Glaucoma?, Glaucoma Australia, viewed 3 July 2024,https://glaucoma.org.au/what-is-glaucoma/types-of-glaucoma/
- Glaucoma Australia 2017a, What Is Glaucoma?, Glaucoma Australia, viewed 3 July 2024, https://glaucoma.org.au/what-is-glaucoma
- Healthdirect 2019, Glaucoma, Healthdirect, viewed 1 July 2022, https://www.healthdirect.gov.au/glaucoma
- Vision Australia 2017, Glaucoma, Vision Australia, viewed 3 July 2024, https://www.visionaustralia.org/information/eye-conditions/glaucoma
- Vision Eye Institute 2024, Glaucoma, Vision Eye Institute, viewed 3 July 2024, https://visioneyeinstitute.com.au/services/glaucoma/
 New
New