'Is my baby healthy?'
This is usually the first and most important question parents ask after delivery. Answering that question accurately requires careful observation, thorough examination and, if needed, onward referral for further assessment.
The aim of both the initial examination at birth and the full neonatal examination is to confirm normality, identify any congenital abnormalities and exclude medical concerns. It also gives the midwife a precious opportunity for further health education and parental reassurance (Gantan & Wiedrich 2023).
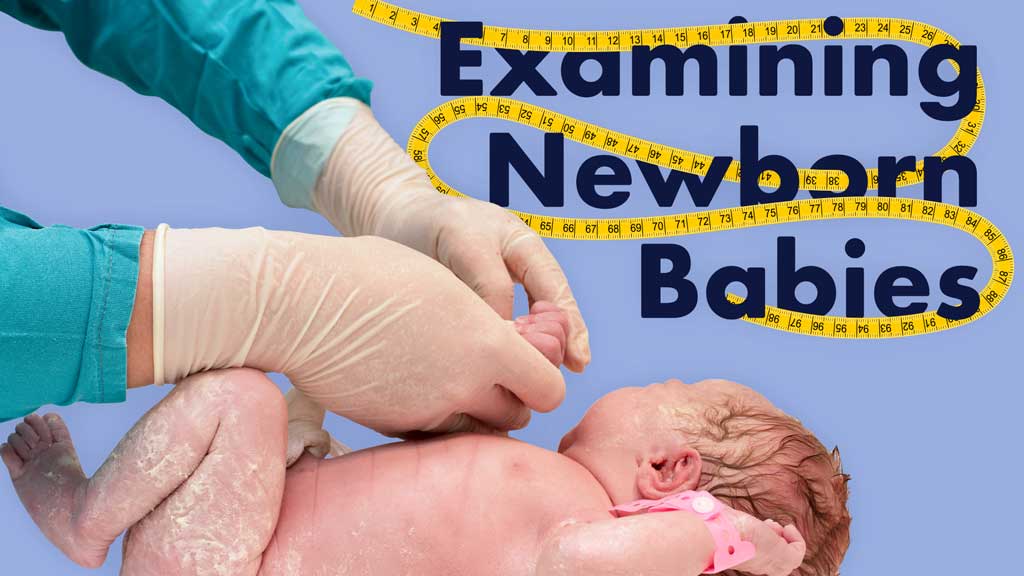
Initial Post-Delivery Assessment and Examination and APGAR Score
Monitoring a successful transition to extrauterine life begins at birth with an assessment of the APGAR score. This is measured at 1, 5, and, if needed, 10 minutes after birth and is followed by an initial examination soon after birth (Pregnancy, Birth and Baby 2023).
| Score of 0 | Score of 1 | Score of 2 | ||
|---|---|---|---|---|
| Appearance | Skin color | Blue or pale all over | Blue at extremities Body pink |
No cyanosis Body and extremities pink |
| Pulse | Pulse rate | Absent | < 100 beats per minute | > 100 beats per minute |
| Grimace | Reflexes and responsiveness | No response to stimulation | Grimace | Cry or active withdrawal |
| Activity | Activity | Limp | Some flexion | Active motion |
| Respiration | Respiratory effort | Absent | Weak, irregular, gasping | Strong, robust cry |
(Pregnancy, Birth and Baby 2023; QAS 2022)
The initial post-delivery assessment aims to exclude obvious abnormalities and includes:
- Assessment of colour to exclude pallor or cyanosis
- Muscle tone, posture and responsiveness
- Heart and respiratory rate
- Normality of facial features, including eyes and mouth
- Normal alignment spine and exclusion of spina bifida
- Genitalia to exclude ambiguity
- Trunk and limbs to exclude obvious abnormality
- Assessment of the anus for patency
- Evidence of birth trauma, such as bruises or scalpel marks.
(Gantan & Wiedrich 2023)
Full Newborn Assessment
This should generally be performed within 48 hours of birth, prior to discharge (Queensland Health 2025).
The aim of this more thorough examination is to:
- Identify acutely unwell newborns who require urgent treatment
- Review and address the family’s concerns about the newborn
- Review suspected or identified issues related to antenatal screening, family history or labour
- Review the newborn’s weight and head circumference
- Assess whether urine and meconium have been passed
- Diagnose any congenital malformations and arrange any required management
- Discuss matters relevant to the newborn (e.g. newborn care, feeding, vitamin K, immunisation, reducing the risk of sudden unexpected death in infancy (SUDI))
- Explain issues such as jaundice that may arise in the following days or weeks
- Discuss local networks, services and access to primary healthcare
- Discuss how the family is able to access additional support if required.
(Queensland Health 2025)
Newborn Screening
Newborn screening involves a heel prick test that is performed 48 to 72 hours after birth. It is used to screen for 25 rare conditions, including:5
- Cystic fibrosis
- Congenital hypothyroidism
- Amino acid disorders
- Organic acid disorders
- Fatty acid metabolism disorders.
(Raising Children Network 2023)
Gathering Relevant Information Prior to Examination
- Anticipated problems based on the maternal and family history
- Factors affecting wellbeing during pregnancy and birth, such as poor fetal growth
- Date, time, type of delivery and birth weight
- Whether the baby has passed urine and meconium.
Prior to the examination, maternal consent should be obtained, the procedure should be explained, and, where possible, the examination should take place at the bedside with the birthing parent present. Including the birthing parent (or both parents if possible) gives the midwife a valuable opportunity to observe the parent(s)' interaction with their baby and address any general concerns they may have.
The Newborn Examination:
- Observe the baby’s general condition, including colour, responsiveness, activity, spontaneous movement, posture and muscle tone. This should be assessed while the newborn is quiet, alert and not hungry or crying.
- Assess the head and skull. Note facial symmetry, fontanelles, sutures, any scalp lacerations or lesions and the presence of any remaining caput, cephalhaematoma or trauma.
- Examine the eyes for size, structure, position and red-eye reflex. Indications for further investigation include a hazy cornea, absent red eye reflex, conjunctivitis, yellow sclera or pupils that are uneven, dilated or constricted.
- Note the position, structure and cartilage of the newborn’s ears. Unresponsiveness to noise, ear drainage or an absent external auditory canal or microtia are indications for further investigation.
- Assess the mouth and palate for size, symmetry, movement, shape and structure. Inspect for craniofacial abnormalities such as a cleft lip or mouth drooping.
- Assess the position and symmetry of the nose (nares and septum).
- Assess the neck for structure, symmetry, range of movement, the thyroid and other masses.
- Check the limbs, hands, feet and digits, assessing proportions, length, structure and symmetry. Examine feet to exclude any postural abnormalities such as talipes.
- Assess the cardiovascular system. Check the newborn’s pulses, perfusion, heart rate, heart rhythm, heart sounds and pulse oximetry.
- Check the lungs. Observe the rate and pattern of chest movement. Listen to the air entry to check for crackles and stridor. Note the presence of any respiratory problems such as tachypnoea at rest, retraction, grunting or nasal flaring.
- Observe the newborn’s abdomen for shape, symmetry and tenderness. Gently palpate to identify any organomegaly, masses or hernia. Confirm the presen.ce of bowel sounds. The condition of the umbilical cord should also be noted.
- Observe the newborn’s genitalia and anus to check for normal appearance, positioning and patency. Check whether the newborn has passed urine and meconium.
- Palpate the testes in male infants for the presence of an undescended position. Cryptorchidism (failure of one or both of the testes to descend into the scrotum) affects approximately 5% of male babies born at term and is associated with a significant increase in the risk of testicular cancer and reduced fertility. Bilateral undescended testes may also be associated with ambiguous genitalia or an underlying endocrine disorder (Yeap et al. 2019).
- Examine the back. Inspect the bony structures and skin of the baby’s spine, with the baby prone. Note the presence of dimples, hair tufts, naevus or abnormal skin patches
- Note the colour and texture of the skin as well as the presence of any birthmarks, rashes, swelling or abrasions.
- Assess the reflexes and central nervous system. Observe tone, behaviour, movements and posture. The grasp, moro and sucking reflexes are assessed.
- Check the hips, symmetry of the limbs and skin folds. Perform Barlow and Ortolani tests to exclude dislocation.
(Queensland Health 2025)
Routine Follow-Up
Parents should be informed that follow-up examinations will be performed at five to seven days of age and again at six weeks of age (Queensland Health 2025).
Test Your Knowledge
Question 1 of 3
Which one of the following findings would necessitate further investigation during a newborn eye examination?
Topics
References
- Gantan, EF & Wiedrich, L 2023, ‘Neonatal Evaluation’, StatPearls, viewed 5 May 2025, https://www.ncbi.nlm.nih.gov/books/NBK558943/
- Pregnancy, Birth and Baby 2023, Apgar Score, Healthdirect Australia, viewed 5 May 2025, https://www.pregnancybirthbaby.org.au/apgar-score
- Queensland Ambulance Service 2022, Assessment/APGAR Score, Queensland Government, viewed 5 May 2025, https://www.ambulance.qld.gov.au/__data/assets/pdf_file/0021/219180/cpp_apgar-score.pdf
- Queensland Health 2025, Newborn Baby Assessment (Routine), Queensland Government, viewed 6 May 2025, https://www.health.qld.gov.au/__data/assets/pdf_file/0029/141689/g-newexam.pdf
- Raising Children Network 2023, Newborn Screening, Raising Children Network, viewed 5 May 2025, https://raisingchildren.net.au/newborns/health-daily-care/health-concerns/newborn-screening
- Yeap, E, Nataraja, RM & Pacilli, M 2019, ‘Undescended Testes: What General Practitioners Need to Know’, Australian Journal of General Practice, vol. 48, no. 1-2, viewed 6 May 2025, https://www1.racgp.org.au/ajgp/2019/january%E2%80%93february/undescended-testes
 New
New