Documentation and Report Writing
How confident are you in your understanding of the critical role of documentation according to the legal requirements of you as a healthcare professional in the Court of Law?
This Ausmed Course will provide an overview of what is considered to be effective communication through documentation in the patient’s record and what adverse outcomes can occur when done poorly.
Content
What you'll learn:
Act on the importance of adequate and accurate documentation to communicate patient information and ensure patient safety.
Use knowledge of judicial interpretation of inadequate documentation to improve communication in patient care records.
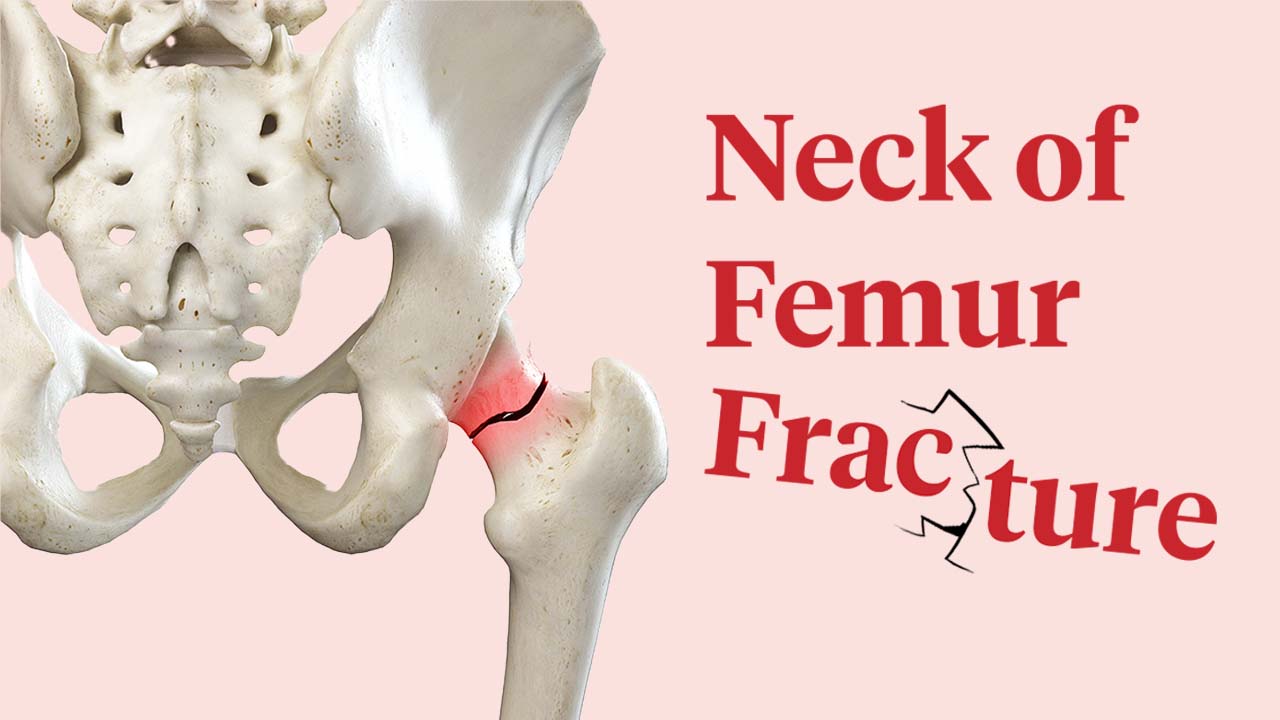
Describe consent requirements for photo/video recording and how the images are incorporated in the patient’s health record to ensure patient rights are protected.
Who it's for:
Why it's needed:
Perhaps the most important role of documentation is to provide a record of continuity of care. In today’s healthcare system, patients are likely to have a range of health professionals providing different aspects of their care. When documentation is done well the patient’s record also serves as an effective tool of communication amongst the team. However, from time to time the patient’s record will be needed in a court or tribunal as evidence in coronial inquiries, criminal or civil matters, or tribunal hearings.
Furthermore, poor documentation can indicate the need for a performance review of the practitioner. As such, it is critical for healthcare professionals to understand how these judicial forums will interpret not only what is written in the record but also what is not and how this may reflect upon them as health professionals and the quality and standard of care they have delivered.
Purpose:
Topics
Assign mandatory training and keep all your records in-one-place.
Find out moreRecommended resources









 New
New