Did you know that urinary catheters are responsible for 80% of healthcare-associated urinary tract infections (SA Health 2024)?
Despite being commonly used, urinary catheters are often inserted unnecessarily and managed poorly, contributing to morbidity and prolonged hospital stays (Gilbert et al. 2018).
Therefore, in order to minimise the risk of complications such as UTIs, the insertion and maintenance of these devices require significant and thorough care from healthcare professionals.
What is a Urinary Catheter?
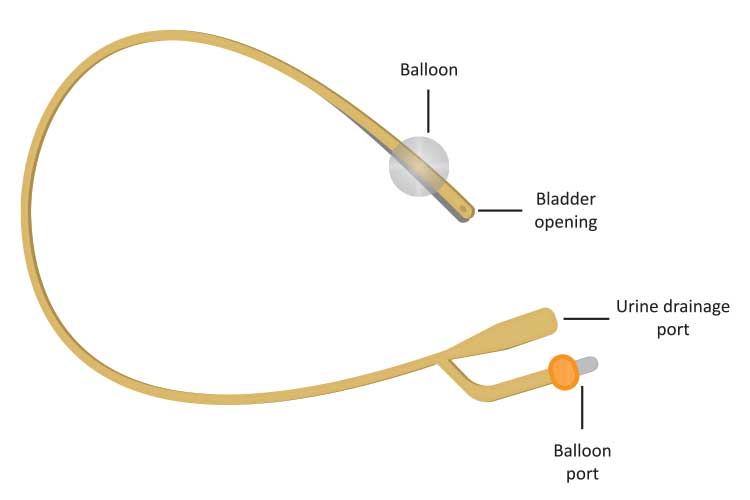
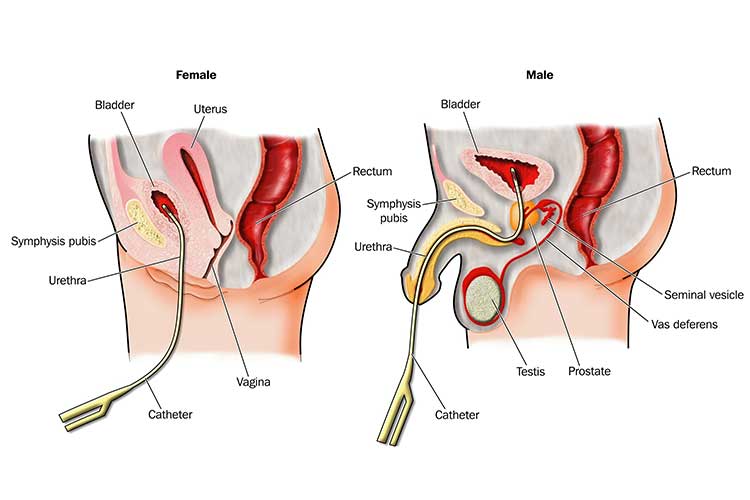
A urinary catheter (also known as an indwelling catheter or long-term catheter) is a hollow, flexible tube inserted through the urethra into the bladder that drains urine into an external collection bag (Cafasso 2023).
Once the catheter has been inserted, a small balloon on the internal end is inflated with sterile water to keep it in situ. The balloon is deflated when the catheter needs to be removed (Cafasso 2023).
Generally, urinary catheters are used by patients who are unable to urinate on their own or have impaired mobility. They are essential in avoiding a build-up of urine, which has the potential to cause pressure in the kidneys and lead to kidney failure (Cafasso 2023).
The process of insertion, known as urethral catheterisation, is invasive and poses significant risks of infection and trauma. Therefore, catheterisations must only be performed by registered nurses or physicians who have undertaken the required qualifications and training (RCHM 2024).
Other Types of Urinary Catheters
There are other types of urinary catheters in addition to indwelling catheters.
- External catheters are non-invasive, condom-like devices that attach to a drainage bag. They are often used by men with urinary incontinence, an overactive bladder, dementia or mobility issues. They are more comfortable and less prone to causing infections.
- Intermittent (‘in and out’) catheters are used to empty the bladder and are then removed. Each time drainage is required, a new catheter is used and then removed. In some cases, the patient can learn to self-catheterise. As these catheters do not stay in situ between drainages, there is less risk of infection or other complications.
- Suprapubic catheters are inserted through the abdominal wall directly into the bladder rather than through the urethra. They are more invasive and require surgical insertion, but they are usually more comfortable for the patient.
(Healthline 2019; Better Health Channel 2021; Jewell 2019; Schaeffer 2024)
Catheter Sizes
Given significant differences in urethral length depending on age and sex, catheters vary in length. Male and female urethras are approximately 20 cm and 4 cm long, respectively (Cadogan 2023).
- Males generally use 41-45 cm catheters.
- Females can use either a 25 cm or 41-45 cm catheter, depending on personal preference.
(Queensland Health 2023)
Patients should use the smallest size catheter appropriate for adequate drainage (Cadogan 2023).
A 12-14 Fr catheter is generally appropriate for both males and females, but a 16-20 Fr catheter may be indicated for patients presenting with debris, mucus, blood clots or haematuria in their urine (Cadogan 2023).
The most appropriate size for paediatric patients will depend on their age, but it is typically between 6 and 10 Fr (RCHM 2024; Cadogan 2023).
Indications for Catheterisation
A patient may have a urinary catheter inserted for the following reasons:
- Urinary retention or obstruction
- Blood clot retention associated with gross haematuria
- Monitoring (sepsis, trauma, renal function, electrolyte or fluid balance)
- Injury or surgery that affects the patient’s urinary function or mobility (e.g. spinal cord injury)
- Investigation, diagnosis or treatment (e.g. bladder irrigation or instillation)
- Urinary incontinence management for wound care, end-of-life care or chemotherapy (only if other available options are too uncomfortable for the patient)
- Urogenital or bladder management (e.g fistula, haematuria).
(CEC 2021)
Caring for and Assessing Urinary Catheters
When caring for a patient with a urinary catheter:
- Ensure that:
- There are no kinks or loops in the drainage bag tubing, and the urine is being continuously drained.
- Both the catheter and drainage device are connected securely.
- The drainage bag is being supported by a stand or hook so that the outlet and tubing are kept off the floor and there are no loops in the tubing.
- The drainage bag is below bladder-level at all times, including during transportation and ambulation.
- The catheter is attached to the patient with a securing device.
- The drainage device is closed unless it is being emptied.
- The drainage bag should be emptied when it is ¾ full, and before any patient transport.
- Before opening the catheter valve, check whether drainage is needed.
- When draining urine, ensure a clean receptacle is used for each patient. Avoid contact between the outlet and the receptacle and clean the outlet with an alcohol wipe afterwards.
- The insertion site should be washed on a daily basis using soap and warm water. Check for discharge, inflammation or ulceration. Antiseptic solutions or ointments should generally be avoided. Dressings are only needed if discharge is present. You should ensure the catheter is secure after washing.
- Males: Wash the meatus, glans penis, catheter and perineum (retracting the foreskin if the patient is not circumcised).
- Females: Wash the urethral meatus, labia minora, catheter and perineum.
- Drainage devices should be changed according to the manufacturer’s recommendations.
- Catheters should only be changed when:
- The closed system has been breached
- The drainage is obstructed
- The patient has a UTI, or
- The catheter has reached its maximum timeframe, as specified by the manufacturer’s instructions.
- The patient’s need for a catheter should be reviewed daily. Ensure the catheter isn't used for longer than necessary to avoid the risk of complications such as infection.
- All catheter care and maintenance, as well as fluid balance charts, should be documented.
(CEC 2021)
The amount of time a catheter can stay in situ may vary. Always refer to the manufacturer’s instructions.

Complications of Urinary Catheters
Catheter insertion is a risky procedure with the potential for a variety of complications. These include:
- Catheter-associated urinary tract infection (CAUTI)
- Decrease in urine output (patient is oliguric)
- Bleeding
- Catheter occlusion
- Urethral trauma
- Displacement
- Incorrect insertion in females (due to difficulty locating the urethral meatus).
(Gilbert et al. 2018; RCHM 2024)
Conclusion
Urinary catheters require thorough assessment and maintenance in order to minimise the risk of infection or injury for patients. It is essential to perform regular daily care, maintain accurate fluid balance documentation and be able to detect and address UTIs or other complications appropriately.
Note: This article is intended as a refresher and should not replace best-practice care. Always refer to your facility's policy on caring for urinary catheters.
Test Your Knowledge
Question 1 of 3
What percentage of healthcare-acquired UTIs is related to urinary catheters?
Topics
Further your knowledge
 Free
Free
References
- Better Health Channel 2021, Urinary Catheterisation, Victoria State Government, viewed 22 May 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/urinary-catheterisation
- Cadogan, M 2023, Urinary Catheterisation, Life in the Fast Lane, viewed 22 May 2025, https://litfl.com/urinary-catheterisation/
- Cafasso, J 2023, ‘Urinary Catheters’, Healthline, 16 November, viewed 22 May 2025, https://www.healthline.com/health/urinary-catheters
- Clinical Excellence Commission 2021, Insertion and Management of Urethral Catheters for Adult Patients, New South Wales Government, viewed 22 May 2025, https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/GL2021_015.pdf
- Gilbert, B, Naidoo, TL & Redwig, F 2018, ‘Ins and Outs of Urinary Catheters’, Australian Journal of General Practice, vol. 47, no 3, viewed 22 May 2025, https://www1.racgp.org.au/ajgp/2018/march/ins-and-outs-of-urinary-catheters
- Healthline Editorial Team 2019, ‘Condom Catheters: How and When to Use’, Healthline, 31 May, viewed 22 May 2025, https://www.healthline.com/health/condom-catheter
- Jewell, T 2019, ‘Suprapubic Catheters’, Healthline, 26 November, viewed 22 May 2025, https://www.healthline.com/health/suprapubic-catheter
- Queensland Health 2023, Urinary Catheter Insertion or Change, Queensland Government, viewed 22 May 2025, https://www.health.qld.gov.au/clinical-practice/guidelines-procedures/clinical-pathways/residential-aged-care-clinical-pathways/all-pathways/urinary-catheter-insertion-or-change#
- Royal Children’s Hospital Melbourne 2024, Indwelling Urinary Catheter - Insertion and Ongoing Care, RCHM, viewed 22 May 2025, https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Indwelling_urinary_catheter_insertion_and_ongoing_care/
- SA Health 2024, Catheter-Associated Urinary Tract Infection Prevention, Government of South Australia, viewed 22 May 2025, https://www.sahealth.sa.gov.au/wps/wcm/connect/public+content/sa+health+internet/clinical+resources/clinical+programs+and+practice+guidelines/infection+and+injury+management/healthcare+associated+infections/indwelling+medical+device+management/catheter-associated+urinary+tract+infection+prevention
- Schaeffer, AJ 2024, Placement and Management of Urinary Bladder Catheters in Adults, UpToDate, viewed 22 May 2025, https://www.uptodate.com/contents/placement-and-management-of-urinary-bladder-catheters-in-adults
 New
New