Multiple sclerosis is the most prevalent acquired chronic neurological disease among young people, affecting over 33,000 Australians in total (MS Australia 2023).
What is Multiple Sclerosis?
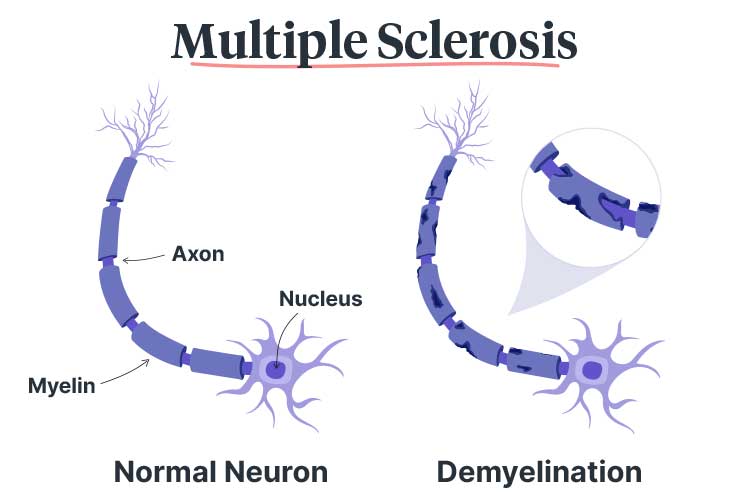
Multiple sclerosis (MS) (which means ‘many scars’) is an incurable neurological condition. It is characterised by an abnormal immune response that targets myelin, a fatty material responsible for insulating the nerve fibres in the central nervous system (CNS) (which comprises the brain, spinal cord and optic nerves) (Better Health Channel 2021).
When the immune system mistakenly attacks the myelin, it is destroyed in a process known as demyelination. This leaves the underlying nerve exposed, leading to inflammation and scarring (lesion formation) (MSRA 2024; Better Health Channel 2021).
This damage disrupts the nerve impulses, impairing their ability to transmit messages between the brain and the body. As a result, the individual will experience a variety of neurological and other symptoms (Better Health Channel 2021).
While the brain will attempt to heal the scarred tissue, some damage may be irreversible. Consequently, the brain will suffer atrophy (loss of volume) (Better Health Channel 2021).
Types of Multiple Sclerosis
MS is an unpredictable disease and may progress differently depending on the individual (Healthdirect 2023).
There are three main clinical courses (‘types’) of MS:
- Relapsing remitting (RMMS): The most common form of MS, accounting for about 85% of initial diagnoses. RMMS causes flare-ups of active disease activity, which are then followed by partial or total remission where the disease does not appear to be worsening. Symptoms may completely disappear during remission periods, or the individual may only partially recover from flare-ups.
- Secondary progressive (SPMS): Occurs when an initial RMMS diagnosis begins to cause progressive worsening of symptoms. Many people with RMMS will eventually develop SPMS, however, this may take several years or even decades.
- Primary progressive (PPMS): Less common. It is characterised by a gradual worsening of symptoms from the onset, causing increased disability. There are generally no remission periods.
(MS Australia 2023; Better Health Channel 2021)
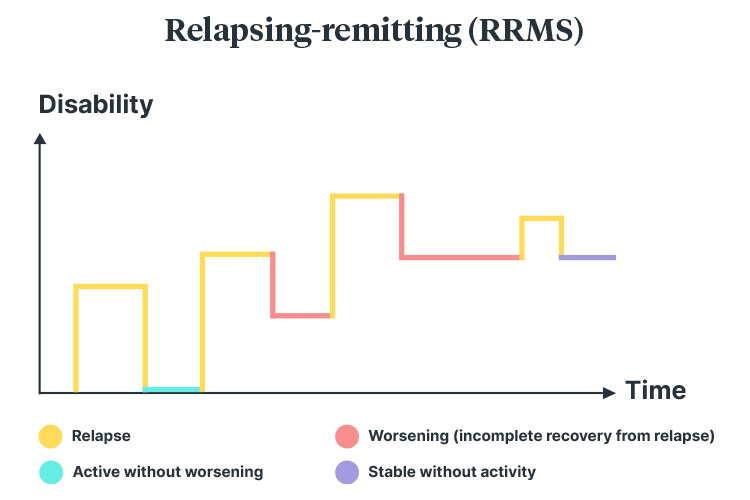
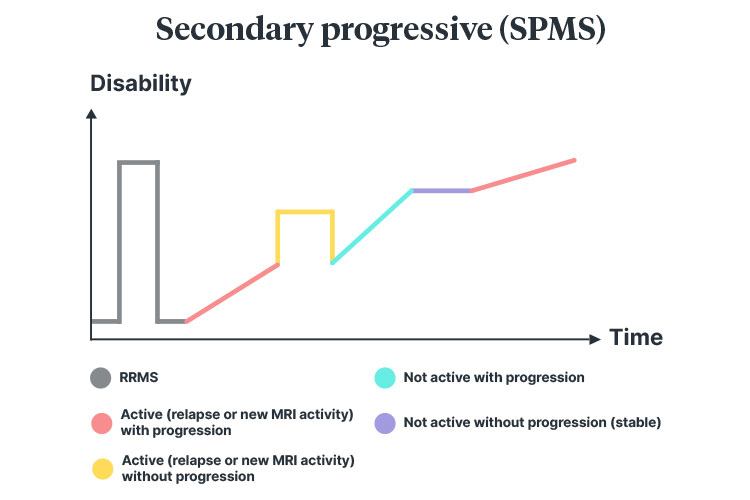
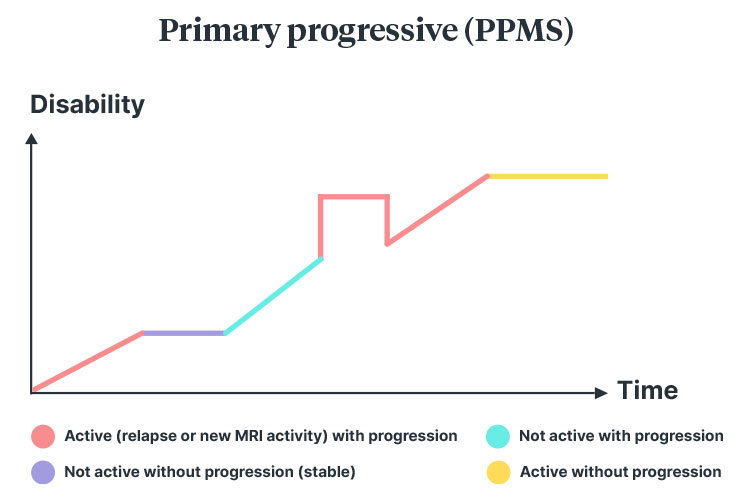
(Diagrams adapted from MS Australia 2023; Lublin et al. 2014)
What Causes Multiple Sclerosis?
A singular cause of MS is unknown, however, it’s believed the condition is linked to an interaction between several factors, including:
- Genetics
- Infection with certain viruses, including Epstein-Barr virus
- Living in an area further from the equator
- Lack of vitamin D
- Smoking.
(MS Australia 2023)
How is Multiple Sclerosis Diagnosed?
A combination of tests is required to diagnose MS, as there is no single diagnostic tool (Healthdirect 2023).
Furthermore, many of the early symptoms, such as fatigue, impaired vision and sensory issues, are non-specific, making diagnosis more difficult (Better Health Channel 2021).
Patients may undergo a variety of tests in order to establish a diagnosis, including:
- Neurological examination
- Blood tests to rule out differential diagnoses
- Magnetic resonance imaging (MRI) to assess for the presence of scarring in the CNS
- Lumbar puncture to assess the cerebrospinal fluid.
(MS Australia 2023)
In order for MS to be diagnosed, there must be evidence of different areas of damage in the CNS that have occurred at different times (Healthdirect 2023).
While it is possible for children to be diagnosed with MS, the majority of people diagnosed are adults between 20 and 40 years of age. About 75% of those living with MS are women (MS Australia 2023).
Symptoms of Multiple Sclerosis
The symptoms of MS vary between individuals and are often unpredictable, with no two cases the same. Generally, symptoms depend on the area of the CNS that has been affected (MS Australia 2023).
The prevalence of depression is three times higher in people living with MS than in the general population, with half of those diagnosed experiencing depressive episodes (MS Australia 2021).
MS Symptoms can be categorised into several areas. People living with MS may experience a combination of the following:
| Motor control symptoms |
|
| Fatigue |
|
| Other neurological symptoms |
|
| Bladder and bowel dysfunction |
|
| Neuropsychological symptoms |
|
(Better Health Channel 2021; MS Australia 2023)
Multiple Sclerosis Relapses
Relapses are characterised by the sudden onset of a new or existing symptom that:
- Lasts for over 24 hours (usually several weeks)
- Has no other clinical explanation apart from MS
- Is separated from a previous attack by more than 30 days.
(MS Australia 2023)
What is the Goal of Treatment for Multiple Sclerosis?
The main treatment for MS is disease-modifying therapies (DMTs), which target the immune system to decrease the frequency and severity of attacks (MS Australia 2023).
There are many different DMTs available in Australia (MS Australia 2023).
As MS is incurable, the main goals of treatment are to maximise the patient’s quality of life by:
- Minimising relapses
- Decreasing inflammation
- Preventing new lesions from forming
- Reducing brain atrophy
- Restoring function
- Reducing the overall impact of symptoms on the patient’s life.
(Better Health Channel 2021)
Other treatments that may help to manage and relieve symptoms include:
- Immunosuppressants, which inhibit the immune system’s activity
- Steroid medicines, which reduce symptoms during a relapse (by decreasing inflammation in affected areas of the body)
- Complementary therapies.
(MS Australia 2023; Better Health Channel 2021)
Patients should also be encouraged to:
- Maintain a healthy weight
- Maintain a healthy diet
- Avoid smoking
- Limit alcohol consumption
- Keep their mind and body active
- Practice stress management techniques (as stress increases the risk of relapse)
- Undergo regular treatment follow-ups, six-monthly treatment reviews and annual MRI scans.
(Better Health Channel 2021)
The Role of the Healthcare Professional in Multiple Sclerosis Care

Treatment of MS may involve an interprofessional team, depending on the patient’s symptoms. The health professionals involved may include:
- Nurses
- MS specialists
- Neurologists
- Physiotherapists
- Occupational therapists
- Continence advisors
- Speech therapists
- Dieticians
- Psychologists or neuropsychologists
- Rehabilitation team
- Pharmacists
- Urologists.
(Multiple Sclerosis Trust 2019; Better Health Channel 2021)
Test Your Knowledge
Question 1 of 3
Finish the sentence: People living with MS are ... as likely to experience depression.
Topics
References
- Better Health Channel 2021, Multiple Sclerosis (MS), Victoria State Government, viewed 14 January 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/multiple-sclerosis-ms
- Healthdirect 2023, Multiple Sclerosis (MS), Australian Government, viewed 14 January 2025, https://www.healthdirect.gov.au/multiple-sclerosis-ms
- MS Australia 2021, Depression, MS Australia, viewed 14 January 2025, https://www.msaustralia.org.au/symptom/depression/
- MS Australia 2023, Understanding Multiple Sclerosis: An Introductory Guide, MS Australia, viewed 14 January 2025, https://www.msaustralia.org.au/wp-content/uploads/understanding-ms_an-introductory-guide_updated-feb-2023_web.pdf
- Multiple Sclerosis Research Australia 2024, What is Multiple Sclerosis (MS)?, MSRA, viewed 14 January 2025, https://msra.org.au/what-is-multiple-sclerosis-ms/
- Multiple Sclerosis Trust 2019, Health Professionals Involved in the Management of MS, MS Trust, viewed 14 January 2025, https://mstrust.org.uk/a-z/health-professionals-involved-management-ms
 New
New 
