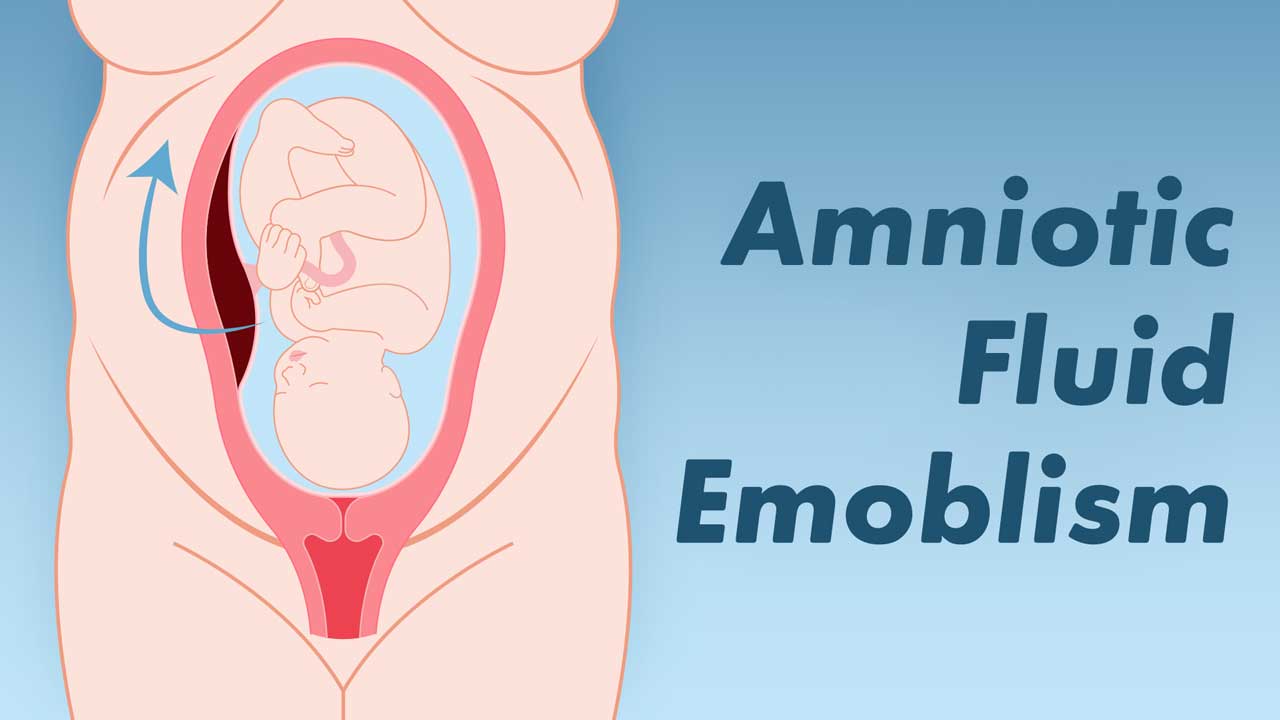
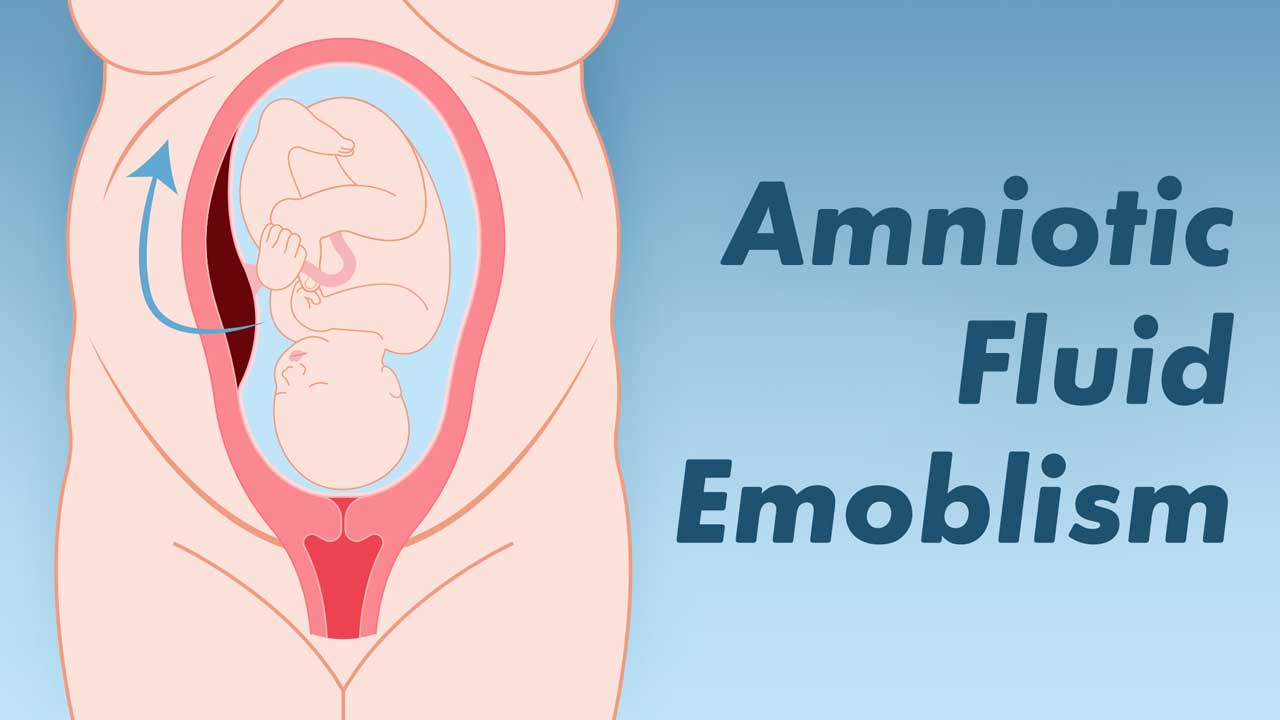
Amniotic fluid embolism (AFE) is a rare, potentially fatal, acute and unexpected birth complication that can affect both the mother and fetus. AFE occurs when amniotic fluid enters the maternal circulatory system and causes an allergic-like reaction (AFE Foundation 2023).
Defined as a two-phase response, AFE is characterised initially by rapid respiratory failure that can then progress to cardiac arrest. The second phase is the haemorrhagic phase, where the birthing parent experiences profuse bleeding at the wound site (usually the site of placental attachment or caesarean incision). Disseminated intravascular coagulopathy (DIC) (also known as consumptive coagulopathy) then develops, which prevents blood clotting. DIC requires urgent transfusions of blood and blood products (AFE Foundation 2023).
Early Warning Signs of Amniotic Fluid Embolism
AFE typically presents during labour or around the time of delivery. Warning signs include a sudden onset of dyspnoea and hypotension, which is often followed by cardiovascular collapse and respiratory arrest. AFE has also been known to occur on rare occasions during first and second-trimester abortions, as late as 48 hours postpartum and following amniocentesis or uterine trauma.
AFE usually develops rapidly with early warning signs that could include:
- Anxiety
- Agitation
- A feeling of doom and panic
- Confusion and altered mental state
- Nausea or vomiting
- Chills
- Skin discolouration
- Breathlessness
- Pins and needles
- Abnormal vital signs.
(AFE Foundation 2023)
This may then lead to more serious symptoms, including:
- Loss of consciousness
- Seizure and/or cardiopulmonary arrest
- Disseminated intravascular coagulopathy.
(AFE Foundation 2023)

Diagnosing Amniotic Fluid Embolism
Diagnosis of AFE is usually made in the absence of other causes. In other words, it is a diagnosis of exclusion made only when all other possible clinical explanations for the symptoms have been ruled out (AFE Foundation 2023).
AFE was originally diagnosed only on post-mortem based on the presence of fetal material found in the vasculature of the lungs, but this is no longer considered a valid diagnostic method (AFE Foundation 2023).
Assessing the Risk of Amniotic Fluid Embolism
Although there is still a great deal of uncertainty about the risk factors related to AFE, potential contributing factors may include:
- Older maternal age
- Multiple pregnancy
- Abdominal trauma
- Undergoing a caesarean birth or operative delivery
- Induction of labour
- Placenta issues (accreta, abruption, praevia)
- Eclampsia
- Tears in the uterus or cervix
- Polyhydramnios
- Uterine rupture
- Assisted fertility
- Early separation of the placenta from the uterus wall.
(Haftel et al. 2024; AFE Foundation 2022; Moldenhauer 2024)
AFE is considered both unpredictable and unpreventable with an unknown cause, which makes risk assessment an almost impossible task. It can occur in healthy patients during labour, during caesarean section, after abnormal vaginal delivery or even during the second trimester of pregnancy (Haftel et al. 2024).

Management of Amniotic Fluid Embolism
Given that AFE cannot be prevented or reversed, treatment of the birthing parent is entirely supportive, focusing on managing individual symptoms as they occur (Haftel et al. 2024).
Initial management should be based on the ABCs of adult life support, prioritising airway, breathing, and circulation (Haftel et al. 2024).
Urgent delivery of the fetus (resuscitative hysterotomy) may be required (Haftel et al. 2024).
Surviving Amniotic Fluid Embolism
AFE is the second most common direct cause of maternal death in Australia (AIHW 2023).
It’s estimated that mortality rate within the first hour after AFE is 50%. Unfortunately, those that survive often experience neurological, pulmonary and cardiovascular impairments (Haftel et al. 2024; Nickson 2020).
Complications after AFE may include, but are not limited to:
- Renal failure
- Cardiac failure
- Respiratory failure
- Heart attack
- Arrhythmias
- Cardiomyopathy
- Congestive heart failure
- Seizures
- Cognitive or neurological impairment.
(Haftel et al. 2024)
The neonatal survival rate is around 70% (Haftel et al. 2024). However, infants who survive may experience cognitive impairment, epilepsy, motor impairment and/or developmental delay due to hypoxic-ischemic encephalopathy (Haftel et al. 2024).
Conclusion
Although AFE cannot be prevented, early diagnosis and intervention may lead to better outcomes for both the birthing parent and the fetus.
As tragic as this condition is, it remains, for the most part, a mystery that can be neither predicted nor prevented.
Topics
References
- Amniotic Fluid Embolism Foundation 2023, What is Amniotic Fluid Embolism?, AFE Foundation, viewed 22 February 2024, https://afesupport.org/what-is-amniotic-fluid-embolism/
- Australian Institute of Health and Welfare 2023, Australia's Mothers and Babies: Maternal Deaths, Australian Government, viewed 23 February 2024, https://www.aihw.gov.au/reports/mothers-babies/maternal-deaths-australia
- Haftel, A, Carlson, K & Chowdhury, YS 2024, ‘Amniotic Fluid Embolism’, StatPearls, viewed 22 February 2024, https://www.ncbi.nlm.nih.gov/books/NBK559107/
- Moldenhauer, JS 2024, Amniotic Fluid Embolism, MSD Manual, viewed 22 February 2024, https://www.msdmanuals.com/home/women-s-health-issues/complications-of-labor-and-delivery/amniotic-fluid-embolism
- Nickson, C 2020, Amniotic Fluid Embolism (AFE), Life in the Fast Lane, viewed 23 February 2024, https://litfl.com/amniotic-fluid-embolism-afe/
 New
New