Low Blood Pressure (Hypotension) Signs and Symptoms
Published: 26 March 2023
Published: 26 March 2023
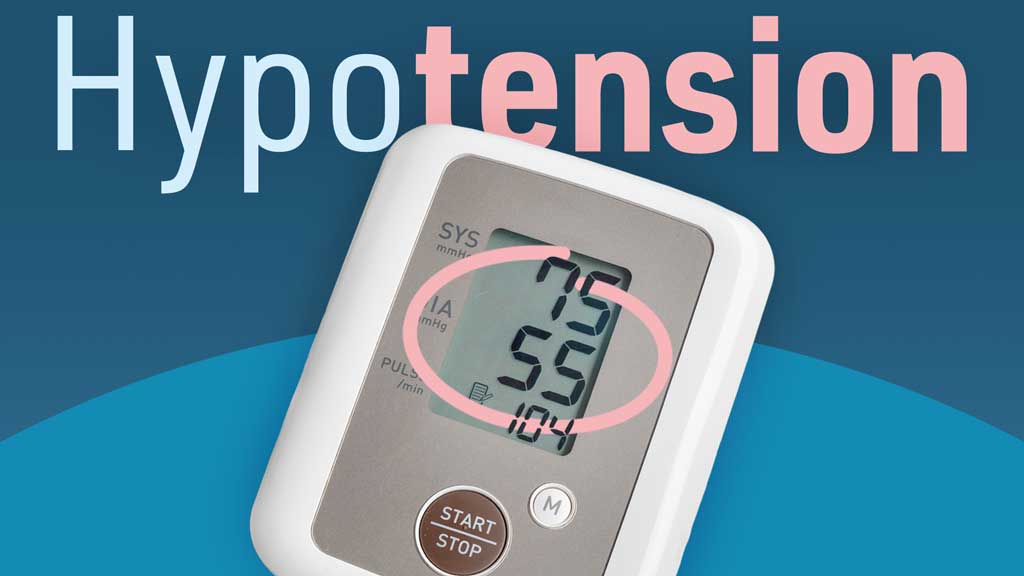
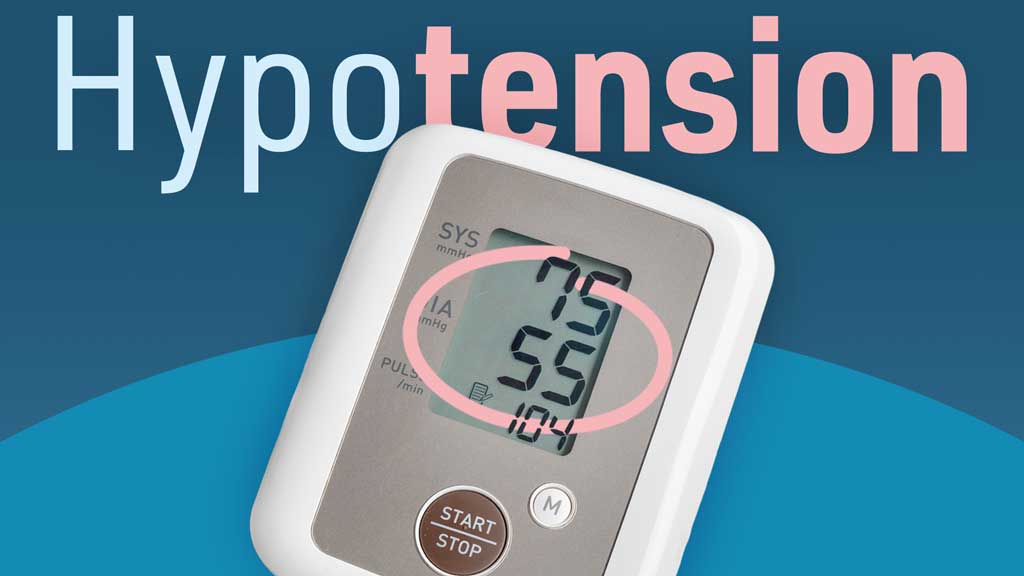
Hypotension (low blood pressure) occurs when the force at which the heart pumps blood through the arteries falls (NHS Inform 2023).
Hypotension can present with various symptoms, from nausea, to dizziness, to heart palpitations (NHS Inform 2023). Checking blood pressure is an important part of evaluating yourself or your patient.
Unfortunately, a problem doesn’t always announce itself with a fanfare of trumpets. Even the highest blood pressure can be entirely asymptomatic. Similarly, low blood pressure can also occur with no symptoms seemingly being present. This is particularly true if the patient is lying still in an unmonitored bed.

In general, hypotension can be thought of as a rate, pump or volume problem. Examples of these include:
Of course, the easiest way to determine whether your patient has a blood pressure problem is by simply taking their blood pressure, but in some cases, you may notice other symptoms that prompt you to check a pressure and find that it is low.
Low blood pressure should be evaluated and treated urgently.
Assessment of a low blood pressure should include a recheck of the pressure and close monitoring. If a client has recently changed positions, they should be returned to a supine position and then rechecked in a few minutes.
The best objective symptom of hypotension is taking the patient’s blood pressure and getting low numbers. It sounds obvious, but it may not occur to you to take a pressure when a patient complains of certain symptoms.
When a patient does complain, however, it is usually recommended that you get a complete set of vitals, and this may then point to a problem with low blood pressure. How low is too low? What does low actually mean? Well, it can mean different things for different patients.
The usual metric for measuring low blood pressure is that anything below 90/60 mmHg (millimetres of mercury) is considered low enough to treat (Healthdirect Australia 2022). Symptoms of low blood pressure can also occur when someone with hypertension comes down from very high pressures. For instance, 120/80 mmHg may be normal for everyone else, but if your patient lives at 170/95 mmHg, they are going to feel the difference. For this reason, the objective sign of a pressure must be combined with the subjective symptoms the patient reports.
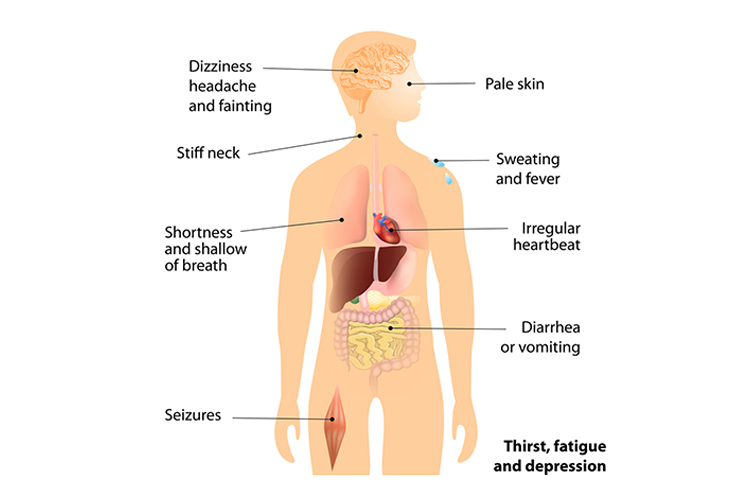
Subjective symptoms are those that the patient may report, though you may be able to see objective signs of these as well.
With low blood pressure, the patient may feel faint or lose consciousness. This is due to lack of blood flow to the brain, and laying the patient supine will usually help to raise blood pressure and reduce symptoms. This could be accompanied by a dizzy feeling and light-headedness (Better Health Channel 2022).
Your patient may also report nausea and could possibly vomit from the low blood pressure. In addition, heart palpitations are sometimes felt, and these can be easily seen with the use of telemetry or other monitoring. EKGs/ECGs may or may not show them, depending on the frequency and timing of the palpitations.
Some patients may also exhibit confusion, and this can make them seem like they are experiencing intoxication or another neurological problem. Blurred vision is usually reported with extreme cases of low blood pressure. There are many other symptoms of low blood pressure to look out for.
Orthostasis means ‘standing upright’. Orthostatic hypotension, or postural hypotension, is defined as a decrease in systolic blood pressure of at least 20 mmHg, or at least 10 mmHg within three minutes of the patient standing. If orthostatic hypotension is present, the patient may be at risk of falls and should be closely supervised with ambulation or advised to call for assistance with activity.
To test for orthostatic hypotension, take the patient’s blood pressure whilst they are supine and at rest. Then stand the patient - they must be able to stand for three minutes before you take their blood pressure again. If the measurements meet the criteria stated previously, then orthostatic hypotension is evident. If the result is equivocal, record it and request a formal assessment.
Question 1 of 3
What kind of problem is a myocardial infarction?