Understanding Malaria: Should Australians be Concerned?
Published: 28 May 2023

Published: 28 May 2023

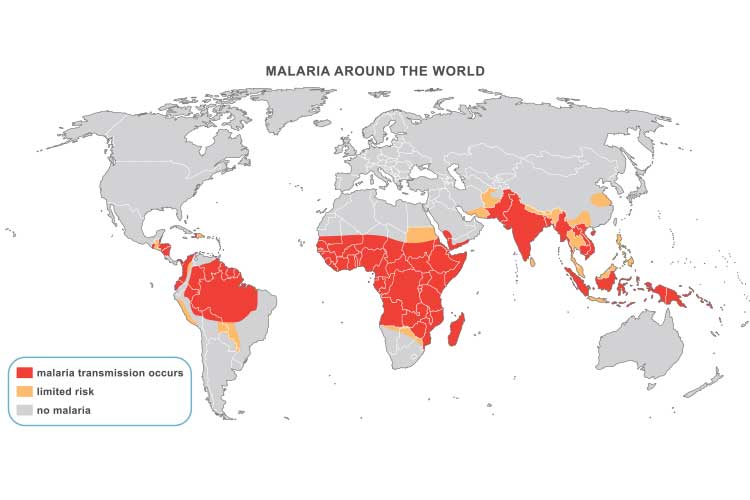
At least 200 million people are infected with malaria every year. In 2021, there were 619,000 malaria deaths worldwide (WHO 2023).
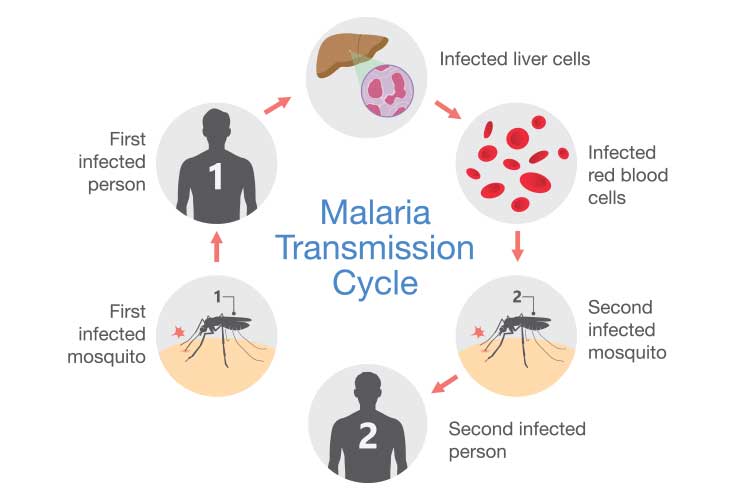
Malaria is an infectious disease caused by the parasite Plasmodium, which is transmitted through the bite of a female Anopheles mosquito. In rare cases, it is transmitted congenitally, via blood transfusion or through shared injecting equipment (WHO 2023a; NSW Heath 2022).
When female Anopheles mosquitoes feed on blood to nurture their eggs, they can pick up Plasmodium parasites from humans infected with malaria. These mosquitoes will then become vectors (carriers) and transmit Plasmodium to other people they bite. You can not contract malaria directly from another person (CDC 2022).
Australia was certified as being malaria-free by the World Health Organisation in 1981 (WHO 2023b).
Despite this, there are still reasons to be vigilant:
(QLD DoH 2022; Healthdirect 2022; Canna 2019)
If Australia is to remain free of malaria, it is imperative that all cases are diagnosed and treated appropriately. Anyone who has been in an area where malaria has occurred within the previous 12 months and who develops a fever should be checked for malaria, both for their own sake and to prevent malaria from getting into the community.
There are five main species of Plasmodium that cause malaria in humans. They differ somewhat in areas where they mainly occur, the symptoms they cause, and treatment required.
(MyDr 2018; Stanford Health Care 2019; WEHI 2023)
After being bitten by an infected mosquito, Plasmodium parasites enter the person’s liver, where they begin to multiply. After a number of days (depending on the type of Plasmodium), the parasites re-enter the bloodstream, invade red blood cells and repromalaria duce (WEHI 2023).
The initial flu-like symptoms are likely to include:
(NSW Health 2022; SA Health 2022)
P. malariae may persist for several years and has been associated with nephrotic syndrome in children (Langford et al. 2015).
Severe malaria may cause symptoms such as:
(UpToDate 2023)
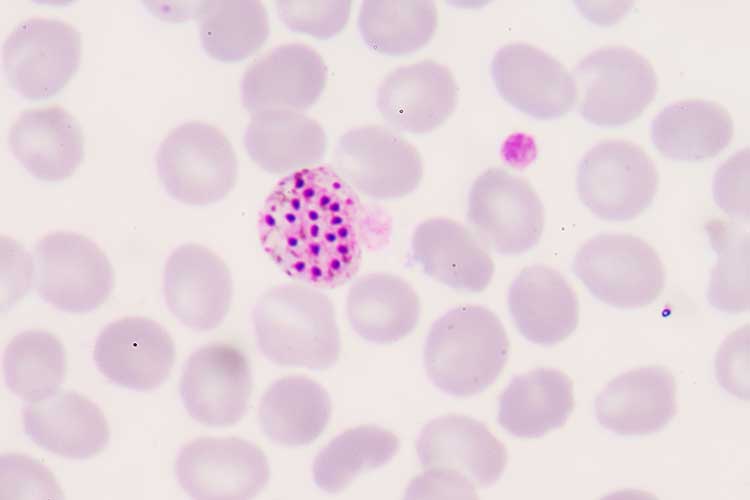
Laboratory diagnosis of malaria is by microscopy. A blood specimen is spread as a smear and examined to confirm the presence of Plasmodium and calculate the percentage of red cells containing the parasites (PHLN 2018).
Malaria is treated with antimalarial medicines to kill the Plasmodium parasites. The exact medicine will depend on factors such as the species of Plasmodium involved, the severity of symptoms, the age of the patient and pregnancy (Mayo Clinic 2023).
Note that there is increasing resistance to antimalarials, so it’s recommended that treatment is overseen by an infectious disease specialist or other expert (SA Health 2022).
Cases of severe malaria require intravaneous administration of antimalarials. If the attack is not classified as severe, oral medications may be used (Buck & Finnigan 2023).
P. vivax and P. ovale may have dormant stages (hypnozoites) that persist in the liver and are not killed by the medication used for the acute attack. The patient may need to take primaquine to eradicate these dormant parasites (Buck & Finnigan 2023).
Anyone travelling to a malarious region should take precautions. This includes consulting a physician to prescribe preventative antimalarial drugs (NSW Health 2022).
No antimalarial drug is 100% effective, so taking precautions to avoid mosquito bites is also crucial. These include:
(NSW Health 2022; Better Health Channel 2015)
Question 1 of 3
True or false: Malaria can be contracted from another person.