The Aged Care Quality and Safety Commission (the Commission) is the cornerstone for safeguarding quality and safety in Australia's aged care sector. Its role is defined by a network of legislative frameworks, including the Aged Care Act 1997, the Aged Care Quality and Safety Commission Act 2018, and associated Rules. This guide outlines the Commission's multifaceted approach to aged care compliance, aiming to boost consumer trust and elevate service quality across the board.
In essence, each assessor has a unique perspective. While they all adhere to the same regulatory guidelines, their interpretations can vary. What one deems compliant, another might not.
The Aged Care Commission's Core Objectives
The Aged Care Quality and Safety Commission (hereafter "the Commission") serves as a regulatory body with key objectives. Its primary role centres on safeguarding the well-being of aged care consumers.
The Commission's objectives are:
- Uphold and Improve: The Commission strives to enhance the safety, health, and overall well-being of those utilising aged care services.
- Boost Confidence: One of the Commission's aims is to instil public trust in the aged care system.
- Facilitate Engagement: Through proactive communication, the Commission seeks to build a dialogue between aged care providers and their consumers concerning the quality of care.
What's the Aged Care Commission’s Scope of Regulatory Powers
The Commission operates under the authority of the Commission Act and the Aged Care Act. Its regulatory functions are both comprehensive and versatile, designed to holistically address the complex landscape of aged care.
The Commission's scope is as follows:
| Area | Explanation |
|---|---|
| Screening Entities: |
Before approval, entities are vetted to ascertain their suitability in offering aged care services. |
| Education: |
Informative resources and support are provided to both consumers and aged care service providers. |
| Addressing Grievances: |
A system is in place to resolve complaints and disputes. |
| Performance Assessment: |
Regular evaluations are conducted against established Aged Care Quality Standards. |
| Monitoring Compliance: |
Activities extend to oversight of Prudential Standards and responsibilities of home care providers. |
| Serious Incident Response: |
Reportable incidents are dealt with under the Serious Incident Response Scheme. |
| Targeted Actions: |
The Commission can take enforcement actions for non-compliance. |
| Data Publication: |
Metrics indicating performance are publicly disclosed. |
Who Does the Aged Care Quality and Safety Commission Act apply to?
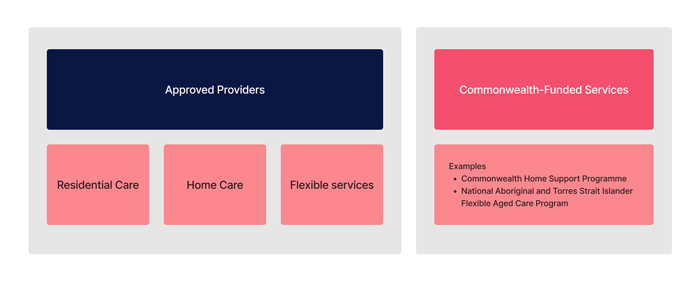
The Commission's policy on compliance and enforcement pertains to a variety of service providers within the aged care sector:
- Approved providers offering residential care services.
- Approved providers offering home care services.
- Approved providers offering flexible care services, including short-term restorative care in residential or home care settings.
- Other Commonwealth-funded services like Commonwealth Home Support Programme services and National Aboriginal and Torres Strait Islander Flexible Aged Care Program services.
How the Aged Care Quality and Safety Commission Identifies Non-compliance
The Aged Care Quality and Safety Commission (the Commission) leverages a diverse set of regulatory tools to scrutinise compliance and pinpoint potential non-compliance. The Commission’s approach is not confined to evidence from a single source; it considers all pertinent evidence for well-rounded decision-making.
Types of Evidence Considered
Evidence comes from a plethora of channels, making the Commission’s evaluations both comprehensive and robust. These include:
- Performance reviews stemming from site audits, quality audits, and assessment contacts.
- Monitoring activities for gauging the quality of care and services.
- Consumer complaints and feedback.
- Requested information from providers.
- Reportable incidents and self-reporting mechanisms.
- Data analysis involving financial records.
- External intelligence, including referrals and publicly disclosed information.
What's the role of the 'decision-maker'?
The decision-maker plays a critical role in assessing all relevant facts and shaping them into logical conclusions. The ultimate question to be addressed is whether the provider has failed to meet one or more responsibilities, substantiated by logically supporting material.
Steps After Identifying Potential Non-Compliance
When initial signs of non-compliance emerge, the following steps may be taken to gather additional evidence:
- Engaging in dialogue with the provider about specific concerns.
- Formally requesting more information from the provider.
- Issuing notices to compel the release of information or documents.
- Initiating additional activities or formal investigations for deeper compliance assessment.
Furthermore, the Commission can conduct site visits either with the provider's consent or through a warrant if needed.
What Actions Can the Aged Care Commission Take to Enforce Non-compliance?
If an organisation fails to meet its responsibilities, the Commission has an array of tools at its disposal for corrective action:
| Action | Explanation |
|---|---|
| Monitoring: |
Regular inspections can be carried out to assess compliance. |
| Public Disclosure: |
Information about non-compliance can be published. |
| Directives: |
Providers may be instructed to implement improvements. |
| Legal Obligations: |
Documents and evidence may be required from providers. |
| Infringement Notices: |
Monetary penalties can be imposed. |
| Legal Action: |
Civil proceedings can be initiated for non-compliance. |
| Sanctions: |
Penalties can be imposed, including revocation of approvals. |
How does the Aged Care Commission determine non-compliance?
Legal Framework for Compliance
Approved providers are governed by responsibilities set forth in Chapter 4 of the Aged Care Act. Any violation activates the Commission's compliance protocols, detailed under Part 7B of the Commission Act, and enforcement powers delineated in Part 8A of the Regulatory Powers (Standard Provisions) Act 2014.
Criteria for Taking Compliance Actions
Before initiating any compliance action, the Commission must be convincingly assured that the provider has failed to meet one or more of its outlined responsibilities. A non-compliance finding is factually substantiated through relevant information (as mentioned in the 'Types of Evidence Considered' section).
How does the Aged Care Commission respond to non-compliance?
The Regulatory Pyramid: A Structured Response Model
The Commission employs a 'Regulatory Pyramid' as a framework for action. At its base are cooperative methods, with more assertive and targeted measures situated at the top. The action taken depends on the provider's willingness and ability to comply. Providers that display negligence or intentionally dodge compliance face stricter measures.
Addressing Systemic Non-Compliance: A Targeted Strategy
In instances of high-impact, widespread non-compliance, the Commission adopts a more focused approach. This can range from targeted actions against a single provider with multiple non-compliant services to broader sector-wide campaigns. Enforceable undertakings serve as an effective tool to hold providers accountable.
Non-Compliance in Reporting: Risk-Based Responses
Providers must meet certain reporting obligations under the Aged Care Act. Failure to comply can result in an array of escalating regulatory actions. The Commission evaluates these instances on a risk-basis, considering factors like the frequency of non-reporting and its potential impact on consumer safety.
What Can Aged Care Providers Do to Meet Compliance to Meet the Aged Care Commission Requirements?
Ensuring compliance within the aged care sector is essential for the well-being and safety of consumers. Providers have multiple roles in this complex process, ranging from adhering to legislative guidelines to the internal monitoring of quality and safety. Here are some key strategies to help providers maintain compliance.
| Strategy | Explanation |
|---|---|
| Understand Legal Requirements |
First and foremost, providers need to be well-versed in the applicable laws and regulations such as the Aged Care Act, the Commission Act, and any other relevant rules. Regular updates on legislative changes are crucial to avoid inadvertent non-compliance. |
| Implement Robust Internal Systems |
The establishment of strong governance and management systems can significantly help in monitoring compliance. These systems should include clear guidelines, checklists, and auditing procedures. Staff training is equally crucial to ensure everyone is aware of compliance requirements. This can be achieved with an Learning Management System (LMS) for aged care. |
| Risk Assessment |
Risk assessment tools should be employed to identify areas of potential non-compliance. A proactive approach in identifying vulnerabilities can aid in prevention rather than cure. Regular reviews should be conducted to reassess and mitigate risks. |
| Consumer-Centric Approach |
Always prioritise the well-being, safety, and quality of life of the consumers. Their feedback should be regularly sought and acted upon, as it serves as a valuable indicator of your performance from a compliance standpoint. |
| Maintain Accurate Records |
Thorough documentation can prove to be invaluable when it comes to proving compliance. From consumer records to staff training documents, maintaining a comprehensive and easily accessible record can facilitate internal reviews and respond effectively to external audits. |
| Engage with Regulatory Bodies |
Actively engaging with regulatory bodies like the Aged Care Quality and Safety Commission can offer you insights into best practices and updates on new guidelines or tools that can assist in maintaining compliance. |
| Periodic Audits and Reviews |
Regular internal and external audits can serve as a wake-up call for any inadvertent lapses in compliance. Immediate corrective action should be taken to address any gaps identified during these audits. |
| Staff Training |
Continual staff training is essential to ensure that all employees are updated on the latest compliance requirements and understand the implications of non-compliance. This training is often referred to as mandatory training. |
| Reporting and Accountability |
Maintain a strict reporting schedule to fulfil your obligations under the Aged Care Act. Transparency in reporting will aid in building trust with regulatory bodies and can serve as evidence of your commitment to compliance. |
Want to engage with members of the Aged Care Quality and Safety Commission?
The Aged Care Quality and Safety Commission is attending Ausmed’s Elevate ’23 Conference and will be available to engage with Providers.
Summary
To summarise, the Commission takes a comprehensive, risk-based approach to addressing non-compliance, relying on a variety of regulatory tools. Providers can ensure compliance by adopting a robust internal framework that includes regular training, transparent reporting, and risk assessments. Adhering to these best practices enables providers to align with Commission requirements and safeguard consumer welfare, ultimately fostering a culture of quality and safety within Australia's aged care sector.
Need a system to support meeting compliance requirements in aged care?
Contact Ausmed today and see how we can support your aged care organisation today!
Additional resources
References
- Aged Care Quality and Safety Commission, ‘Compliance and enforcement policy’, https://www.agedcarequality.gov.au
- Australian Government, 'Aged Care Act 1997', Federal Register of Legislation, https://www.legislation.gov.au/Series/C2004A05214
- Australian Government, 'Aged Care Quality and Safety Commission Act 2018', Federal Register of Legislation, https://www.legislation.gov.au/Series/C2018A00149
- Aged Care Quality and Safety Commission, Regulatory pyramid infographic Nov 2022, https://www.agedcarequality.gov.au/media/94534