This article is part of our Training Requirement Series where we provide comprehensive guides to meet the actual training requirements that are often needed/requested of learning and development departments within Australia's healthcare organisations. This series includes both general requirements, such as healthcare rights and informed consent but also focuses on the specific requirements stemming from the NDIS, Aged Care and NSQHS Quality Standards.
What is Healthcare Rights?
Healthcare rights in Australia encompass the right to access, safety, respect, communication, participation, privacy, and comment. These rights ensure that care is safe and of high quality. The Australian Charter of Healthcare Rights provides a framework for ensuring patients' rights are respected and upheld.
What is Informed Consent?
Informed consent is a process where a healthcare provider educates a patient about the risks, benefits, and alternatives of a proposed procedure or intervention. The patient must understand and voluntarily agree to the treatment. Informed consent is both an ethical obligation and a legal requirement, integral to patient autonomy and decision-making.
Importance of Healthcare Rights and Informed Consent
Understanding and upholding healthcare rights and obtaining informed consent are vital. They ensure ethical practice, promote patient safety, and reduce legal risks. Adherence to these principles is essential for building trust and effective communication between healthcare providers and patients.
What is the "Healthcare Rights and Informed Consent" Training Requirement?
Training in healthcare rights and informed consent is mandated by Australian healthcare standards. It ensures that staff are competent in understanding patients' rights, ethical considerations, and legal requirements associated with informed consent.
Relevant Standards
The health organisation has a charter of rights that:
- a) Is consistent with the Australian Charter of Healthcare Rights
- b) Is Easily accessible for patients, carers, families and consumers
The health organisation ensures that its processes of informed consent comply with best practice and legislation
The health organisation has processes to identify:
- a) The capacity of a patient to make decisions about their own care
- b) A substitute decision maker if a patient does not have the capacity to make decisions for themselves
National Safety and Quality Health Service (NSQHS) Standards
Action 1.3.2: Informed consent
The provider implements a system to ensure that older people give their informed consent where this is required for a treatment, procedure or other intervention.
Action 1.4.4: Transparency - Client fee changes
The provider informs the older person of any changes to previously agreed fees and charges and seeks their informed consent to implement these changes before they are made.
Action 2.7.2: Transparency - Client fee changes
The provider’s information management system ensures that:
- d. older people understand their right to access or correct their information or withdraw their consent to share information
Action 3.1.2: Communicating assessment and planning outcomes to clients
The outcomes of assessment and planning are effectively communicated to:
- a. the older person, in a way they understand
- b. the older person’s family, carers and others involved in their care with their informed consent.
Strengthened Quality Standards framework analysis - Aged Care Quality Standards
Failure to comply with the requirements could lead to an organisation being penalised or reprimanded.
Related Training Requirements Guides
The following Training Requirement guides can be used to support and facilitate the "healthcare rights and informed consent" training requirement:
Skills Required for Healthcare Rights and Informed Consent
Proficiency in healthcare rights and informed consent is foundational for healthcare professionals. The following skills are critical for ensuring that patients receive care that is not only clinically appropriate but also ethically sound and legally compliant.
- Effective Communication: Clear and empathetic communication with patients.
- Empathy and Patient Engagement: Understanding patient perspectives and concerns.
- Legal Knowledge: Familiarity with healthcare standards and legal requirements.
- Ethical Decision-Making: Navigating ethical dilemmas in patient care.
- Documentation and Record-Keeping: Accurate and thorough documentation practices.
How to Assess Staff Competency in Healthcare Rights and Informed Consent
Regular assessment of staff competency in healthcare rights and informed consent ensures that healthcare professionals remain equipped to handle the complexities of patient care. The following methods can be employed:
- Role-playing Exercises: To simulate real-world scenarios.
- Written Assessments: To test knowledge and understanding.
- Practical Demonstrations: To observe skills in action.
- Regular Performance Reviews: To provide ongoing feedback and guidance.
Strategies to Support Healthcare Staff Develop Skills in Healthcare Rights and Informed Consent
Developing skills in healthcare rights and informed consent requires a multi-faceted approach. Effective training strategies can include:
- Workshops: Interactive sessions focusing on communication and legal aspects.
- E-Learning Modules: For flexible, self-paced learning.
- Scenario-Based Learning: Hands-on approach using practical examples.
- Mentorship and Support Sessions: Ongoing guidance and support for continuous improvement.
Sample Training Plan for the Healthcare Rights and Informed Consent Requirement
A structured training plan is essential for developing quality improvement skills.
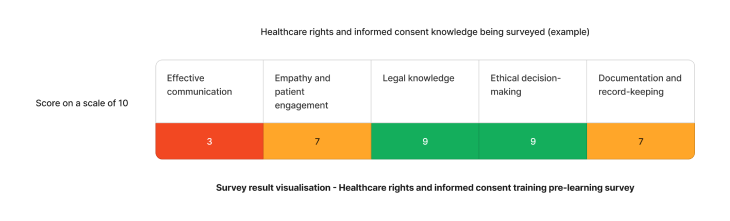
Using the above needs assessment survey as an example - The skill requiring the most attention for healthcare rights and informed consent are communication skills. We can target learning initiatives to fill these gaps to enhance staff competency.
Need an LMS that can support healthcare rights and informed consent?
Contact Ausmed today and see how we can support with your training requirement needs!
Staff Competency Assessment for Healthcare Rights and Informed Consent - Example
To evaluate an individual's skills in healthcare rights and informed consent, consider using these survey questions:
Staff Survey - Healthcare Rights and Informed Consent Competency
-
How would you explain informed consent to a patient?
- [Answer here]
-
How would you handle a situation where healthcare rights are at risk?
- [Answer here]
-
What are your steps when a patient refuses treatment?
- [Answer here]
-
What are the key components of informed consent?
- [Answer here]
-
Describe how you ensure adherence to healthcare rights in practice.
- [Answer here]
-
Recall a challenge in obtaining informed consent and your response.
- [Answer here]
Conclusion
In conclusion, training in healthcare rights and informed consent is essential for the delivery of high-quality patient care. Through thoughtful training programs and continuous skill development, healthcare professionals in Australia can ensure adherence to both the ethical and legal standards of patient care.
References
- Australian Commission on Safety and Quality in Health Care, 2023. 'Partnering with Consumers Standard'
- Australian Commission on Safety and Quality in Health Care, 2023. 'Australian Charter of Healthcare Rights'
- Australian Commission on Safety and Quality in Health Care, 2023. 'NSQHS Action 2.03'
- Australian Commission on Safety and Quality in Health Care, 2023. 'NSQHS Action 2.04'
- Australian Commission on Safety and Quality in Health Care, 2023. 'NSQHS Action 2.05'
- Aged Care Quality and Safety Commission, 2023. 'Stronger Standards, Better Aged Care Program - Action 1.3.2, 1.4.4, 2.7.2 (d), 3.1.2'