This article is part of our Training Requirement Series where we provide comprehensive guides to meet the actual training requirements that are often needed/requested of learning and development departments within Australia's healthcare organisations. This series includes both general requirements, such as optimising and conversing patients' own blood but also focuses on the specific requirements stemming from the NDIS, Aged Care and NSQHS Quality Standards.
What is Optimising and Conserving Patients' Own Blood in Healthcare Organisations?
Optimising and conserving patients' own blood involves a range of strategies aimed at identifying and managing patients who are at risk of blood loss in a healthcare setting. Early identification will reduce the need for transfusions, thereby preserving the patient's own blood. These strategies include preoperative optimisation of haemoglobin levels, minimising blood loss during surgery, and enhancing postoperative red cell mass recovery.
What is the "Optimising and Conserving Patients’ Own Blood" Requirement?
The optimising and conserving patients’ own blood requirement, as outlined under the National Safety and Quality Health Service (NSQHS) Standards, specifically Action 7.04, mandates healthcare organisations to implement systems aimed at maximising the patient's own blood use and conserving it wherever possible. This directive underscores the critical importance of managing a patient's blood as a precious resource, focusing on reducing the need for blood transfusions by enhancing and preserving the patient's endogenous blood supply.
Relevant Standards
Clinicians use the blood and blood products processes to manage the need for, and minimise the inappropriate use of, blood and blood products by:
- a) Optimising patients’ own red cell mass, haemoglobin and iron stores
- b) Identifying and managing patients with, or at risk of, bleeding
- c) Determining the clinical need for blood and blood products, and related risks
Clinicians use the safety and quality systems from the Clinical Goverenance Standard when:
- a) Implementing policies and procedures for blood management
- b) Managing risks associated with blood management
- c) Identifying training requirements for blood management
National Safety and Quality Health Service (NSQHS) Standards
Failure to comply with the requirements could lead to an organisation being penalised or reprimanded.
Related Training Requirements Guides
The following Training Requirement guides can be used to support and facilitate the blood management events training requirement:
Why is Optimising and Conserving Patients' Own Blood Important?
Optimising and conserving patients' own blood is vital for improving clinical outcomes, reducing the risks associated with blood transfusions, and ensuring the sustainable use of blood resources. It is crucial for patient safety, healthcare efficiency, and aligns with the principles of patient-centred care.
- Improvement of Clinical Outcomes: Conserving a patient's own blood can lead to better recovery rates, fewer complications, and shorter hospital stays.
- Reduction in Transfusion Risks: By minimising the need for blood transfusions, the risks of transfusion-related reactions, infections, and alloimmunization are significantly reduced.
- Enhanced Patient Safety: Optimising a patient’s blood volume and quality before, during, and after surgery reduces the likelihood of adverse events and promotes overall patient safety.
- Resource Sustainability: Using blood conservation techniques helps in managing the blood supply more efficiently, ensuring that these critical resources are available for those in dire need.
- Cost Efficiency: Reducing the dependence on blood products can also lower healthcare costs related to procurement, storage, and transfusion of blood.
- Alignment with Patient-Centred Care: It respects patient preferences, especially those who decline blood transfusions for personal or religious reasons, and supports the right to self-determination in healthcare decisions.
- Compliance with Healthcare Standards: Adhering to blood conservation practices aligns with national and international guidelines and standards, promoting best practices in patient care.
What Skills do Staff Need for Optimising and Conserving Patients' Own Blood?
Staff involved in patient care require a specific set of skills to effectively contribute to blood conservation efforts. These skills include:
| Skill | Relevance |
|---|---|
| Understanding of blood conservation principles and techniques | This skill involves knowledge of the various strategies and practices aimed at reducing blood loss and avoiding unnecessary transfusions. It includes familiarity with guidelines. |
| Optimise patient haemoglobin levels preoperatively | Evaluate a patient's blood count and iron status before surgery and take steps to correct any deficiencies. |
| Minimise invasive surgical techniques | These techniques generally lead to less blood loss, shorter hospital stays, and quicker recoveries. Staff need to be skilled in these techniques to effectively reduce intraoperative blood loss |
| Risk Management and Safety Awareness | Professionals need to understand the risks associated with blood transfusion and blood product management, including the ability to implement safety protocols to minimise these risks. |
| Proficiency in blood loss monitoring and management during procedures | Accurately estimate blood loss in real time and implement immediate measures to manage significant bleeding. |
| Postoperative patient monitoring and care to support blood volume recovery | monitor patients for signs of anemia or blood loss and to manage their recovery to promote red blood cell regeneration and blood volume restoration. |
How to Assess Staff Competency in Blood Optimisation and Conservation?
To ensure staff are competent in patient blood conservation, healthcare organisations should implement a structured competency assessment framework.
This framework may include:
- Self-Assessment Tools: Encouraging staff to evaluate their own knowledge and skills in reporting adverse events, helping identify areas for improvement and personal development.
- Feedback from colleagues: Gathering insights from peers regarding the staff's performance and ability to handle adverse events, providing a well-rounded view of their competencies..
- Simulations exercises: Test decision-making and procedural skills in controlled environments.
- Case Study Analysis: Utilise real-world scenarios to test staff's ability to apply their knowledge and skills in practical settings, encouraging critical thinking and problem-solving.
- Competency Checklists: Develop detailed checklists based on specific roles and responsibilities related to blood management to systematically assess and document competency levels.
- Continuous performance monitoring Monitoring involves regular reviews of staff performance in blood conservation practices.
- Digital Learning Platforms: Utilise technology to present and evaluate training modules, offering a more adaptable and individualised method for assessing competencies.
Strategies to Support Employees Enhance Skills in Patient Blood Optimisation and Conservation
Developing and enhancing staff skills in patient blood conservation can be achieved through a variety of strategies:
- Regular training sessions: These sessions provide continuous learning and upskilling opportunities, focusing on the latest advancements and best practices in blood conservation. They ensure all staff remain knowledgeable and proficient in their roles.
- Mentorship programs: Mentorship programs facilitate knowledge transfer and hands-on learning by pairing novice employees with seasoned professionals. This approach helps to cultivate expertise and confidence in blood conservation practices among newer staff members.
- Access to online resources and continuing education opportunities: Providing staff with access to a wide range of online learning materials and courses allows for self-paced learning and continuous professional development in the field of blood management and conservation.
- Encouragement of interdisciplinary collaboration: Promoting teamwork across different disciplines within the healthcare setting encourages the exchange of ideas and experiences. This collaborative environment supports the dissemination and implementation of best practices in patient blood optimisation and conservation.
After outlining these strategies, it's crucial to understand that enhancing staff skills in patient blood optimisation and conservation requires ongoing effort. Implementing these measures ensures a supportive learning environment, elevates staff competencies, and improves patient care. Regular training, mentorship, accessible resources, and collaboration equip teams to effectively conserve patient blood, leading to better outcomes.
Sample Training Plan for Optimising and Conserving Patients' Own Blood
Below is an extended sample plan:
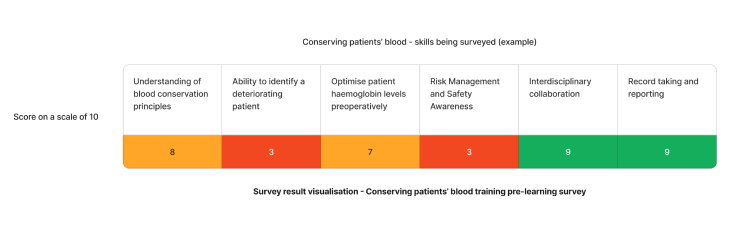
Using the above needs assessment survey as an example - The skill requiring the most attention for reporting adverse blood management events in healthcare are ability to identify a deteriorating patient and risk management and safety awareness. We can target learning initiatives to fill these gaps to enhance staff competency.
Need an LMS that can support training in optimising and conserving patients' own blood?
Contact Ausmed today and see how we can support with your training requirement needs!
Staff Competency Assessment for Optimising and Conserving Patients' own Blood - Example
Consider the following survey questions:
Staff Survey - Assess Optimising and Conserving Patients' Own Blood Competency
-
How confident do you feel in identifying a deteriorating patient?
- [Answer here]
-
Describe a situation where you successfully applied minimally invasive techniques to reduce blood loss
- [Answer here]
-
Have you encountered any challenges in reporting adverse events? If so, please describe?
- [Answer here]
-
In your opinion, what are the key barriers to implementing effective blood conservation measures in our organisation?
- [Answer here]
-
In what ways could the reporting process be improved to facilitate more timely and efficient reporting of adverse events?
- [Answer here]
Conclusion
In conclusion, the development and implementation of a training program focused on optimising and conserving patients' own blood is a crucial step towards enhancing patient safety and care quality within healthcare organisations. It's imperative for healthcare organisations to foster an environment of continuous learning and improvement, ensuring that all team members are competent and confident in their ability to contribute to effective patient blood management.
References
- Australian Commission on Safety and Quality in Health Care, 2024. 'Blood Management Standard'
- Australian Commission on Safety and Quality in Health Care, 2024. 'NSQHS Action 7.04'
- Australian Commission on Safety and Quality in Health Care, 2024. 'NSQHS Action 7.01'
- Goobie, SM, 2022, 'Patient blood management is a new standard of care to optimize blood health, Anesthesia & Analgesia', vol.135, no.3, pp.443-446.
- Ozawa, S, Ozawa-Morriello, J, Rock, R, Sromoski, M, Walbolt, S, Hall, T and Pearse, BL, 2024, 'Patient Blood Management as an Emerging Concept in Quality: The Role of Nurses. Journal of Nursing Care Quality', vol. 39, no.2, pp.129-135.
- National Blood Authority, n.d. Patient Blood Management Guidelines