Structure of the New Standards
Our belief, after careful assessment of the new Strengthened Aged Care Quality Standards, regulatory model, and copious amounts of associated reading material, is that there are significant educational implications related to the new Standards. This is a considerable period for aged care; we all have a duty of care to get this implementation right. The role of L&D is critical. We are here to support you because we believe that education drives change.
This guide offers a detailed explanation of every component of the new Standards. It's crucial for L&D teams to understand the architecture of these standards if they are to plan and implement targeted activities in line with new training requirements and to be well-prepared for assessment at the Outcomes level.
In total, there are seven Strengthened Aged Care Standards, 34 outcomes, and 152 actions across all standards. If we look at the structure of each standard, there are four key elements. Outcomes sit at the core structure of each standard and are the enforceable element, that is, what providers are assessed against.
-1.png)
Intent
Each standard begins with an Intent. Depending on the Standard, an intent can vary between approximately 100-300 words. The intent starts by describing the responsibilities of a provider. It is made clear that the responsibility ultimately lies with the governing body; for example, the purpose of Standard 5 is that the provider delivers safe and quality clinical care to older people. The governing body has overall responsibility to develop and implement a clinical governance framework. The framework must be operationalised and used to measure and report on whether safe and quality clinical care is being provided to older people.
The intent empathises with the older person’s needs to help interpret what someone might be experiencing and validate the need for the standard. For example, older people often have multiple chronic and usually complex comorbidities. Their care needs are complex, and they often concurrently experience sickness, frailty, disability, and cognitive impairment, and this could all occur towards the end of life.
The intent describes the desired outcome of what meeting the standard looks like from the perspective of the person—for example, referring to Standard 5 again. Quality care optimises quality of life, reablement and maintenance of function, and improves health. It explicitly says that what this could look like is an older person being able to continue to participate in an activity that they find enjoyable, that gives them meaning, as a result of being clinically stable and in good enough health.
The intent includes characteristics of what meeting the standard involves. For example, that it is inclusive and safe, and decisions involve family, carers, and the person. The intent makes it clear who is involved in meeting the Standard. For example, Clinical Care (Standard 5) requires a multidisciplinary approach and involves a skilled, competent workforce, including allied healthcare teams, to provide evidence-based, contemporary care.
Expectation Statement
This is a short, person-centred statement that quite explicitly describes, from the older person’s perspective, what precisely an older person expects to receive. For example, the expectation statement for Standard 3, The Care and Services, states that “The care and services I receive are safe and effective, optimise my quality of life, including through maximising independence and reablement, meet my current needs, goals and preferences, are well planned and coordinated and respect my right to take risks”. Our perspective is that this is a beautiful inclusion as it helps us all to really hear the voice of an older person, telling us precisely what they expect.
Outcomes
Collectively, outcomes are the enforceable element, meaning this is what will be the focus of an audit. There are 34 outcomes spread across the seven standards. The number of outcomes ranges between two and ten per standard, so there’s an average of four outcomes per standard. Standard 2, The Organisation, has the highest number of outcomes per standard, 19, with a focus on clinical governance, quality, safety, risk, accountability, and workforce planning and management. Standard 5, Clinical Care, has a total of seven outcomes, detailing the quality care requirements across key areas, including preventing and controlling infections, safe and quality use of medicines, communication, and end-of-life care. Of course, all standards are essential and relate to each other, and success is dependent on all standards being met. In general, the number of outcomes per standard can indicate the depth and resources, activities, and initiatives an organisation may choose to allocate as they work towards full implementation of the Standards.
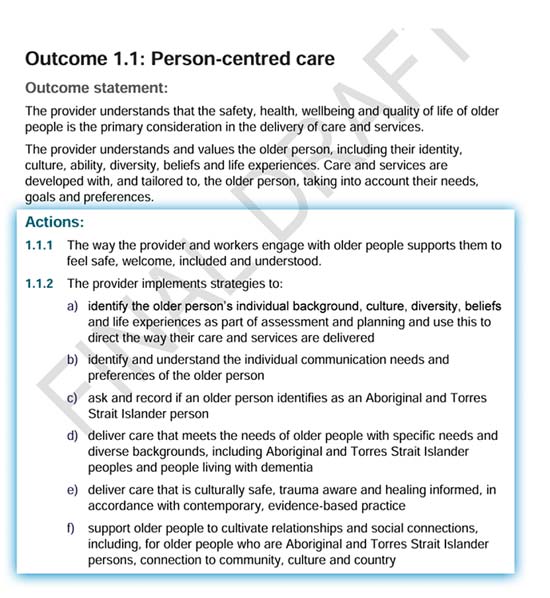
Outcome Statement
Attached to each of the 34 outcomes is an outcome statement. Outcome statements are what providers will be literally assessed against. They are typically two short paragraphs that are very explicit in nature. That is, they set forth precisely what the provider needs to know, show, or do. There's no doubt.
Actions
Actions are how providers might demonstrate the achievement of an outcome. They are more practical, listed step-by-step, and often reference the need to implement a system and have an effective process in place. Within the actions, though, are also apparent educational requirements. Some can be quite specific, for example, ‘The provider implements processes to correctly identify and match older people to their care and services and provide Care Statements.’ Others may leave more room for providers to demonstrate in their own way, tailored to their context and service, how they are achieving the outcome; for example, Action 1.2.3 ‘The relationships between older people and their family and carers are recognised and respected’.
Understanding the fundamental structure of a standard is foundational knowledge for L&D teams. As we head towards July 1 rapidly, we all have to pick up the baton and push change forward. We are all enablers to improve care. Even if we are at a desk, behind a computer, or in a board room, this is an opportunity to enhance older people’s health and lives genuinely. Ausmed is here to support you in using education to drive this change.
References and Resources
- The Strengthened Aged Care Quality Standards – Final draft
- Aged Care Quality Standards: Standard 5 – Clinical Care
- Draft audit methodology
- Draft evidence framework
- Draft pre-audit preparation tool
- Glossary
- Royal Commission into Aged Care Quality and Safety Final Report: Care, Dignity and Respect
- Australian Government Response to the Final Report of the Royal Commission into Aged Care Quality and Safety
- Aged Care Bill 2023 Exposure draft
- New Aged Care Act: Defining high-quality care
- Supporting Sector Readiness for the New Strengthened Aged Care Quality Standards (Webinar)
Author
Zoe Youl
Zoe Youl has over ten years of experience at Ausmed. With expertise in Critical Care Nursing, Clinical Governance and Education, she has built an in-depth understanding of the educational and regulatory needs of the Australian healthcare sector.