Parkinson's Disease
Published: 10 October 2022

Published: 10 October 2022

Parkinson’s disease is a progressive neurological condition, marked by both motor and non-motor symptoms.
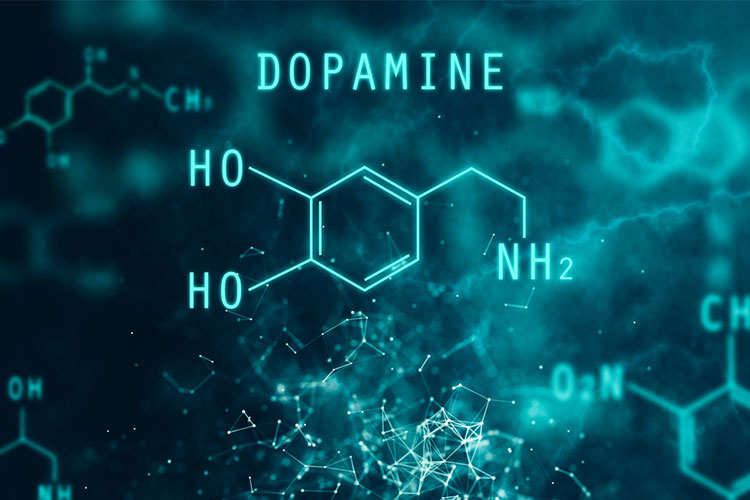
Parkinson’s disease is the result of deterioration occurring in the nerve cells in the middle area of the brain (parietal lobe), the area in which dopamine is produced (Better Health Channel 2020).
Dopamine relays messages between areas of the brain that are responsible for body movement, particularly, the smooth control of muscles and mobility (Brain Foundation 2022; Healthdirect 2021).
Low levels of dopamine make it difficult to manage muscle tension and muscle movement, both at rest and during activity (Brain Foundation 2022).
Parkinson’s is often understood as a ‘movement disorder’ due to its association with tremors, stiffness and balance problems. However, there are many non-movement issues that also occur as a result of this disease. These non-movement symptoms can include depression, constipation and memory loss (Michael J. Fox Foundation 2019).
As Parkinson’s disease is a progressive condition, its symptoms worsen over time (Better Health Channel 2020).
The disease is named after British physician James Parkinson, who first described it in 1817 (Parkinson’s News Today 2021).
It’s estimated that there are close to 219,000 Australians living with Parkinson’s disease (Fight Parkinson’s 2022).
Parkinson’s disease is a global phenomenon, recognised across cultures. It is estimated to impact 8,500,000 people worldwide and is slightly more common in men than in women (WHO 2022; Brain Foundation 2022).
Primarily, Parkinson’s disease occurs in people over the age of 65, but onset can take place earlier (Healthdirect 2021).
About 20% of people with Parkinson's will experience symptoms before the age of 50. This is known as young onset Parkinson's. Treatments are the same but the experience of the disease tends to differ (Parkinson's Australia 2020a; Michael J. Fox Foundation 2016).
The exact cause of Parkinson's disease is not yet understood, hence the name ‘idiopathic Parkinson’s disease’ (Better Health Channel 2020; Parkinson’s Australia 2020b).
However, factors that may contribute to the development of Parkinson’s disease include the following (or a combination of these):
(Parkinson’s Australia 2020b; Better Health Channel 2020)
It is thought that only a small percentage of cases (around 15%) are passed on through genetics (Parkinson’s Australia 2020b).

The symptoms of Parkinson’s disease will vary according to type, severity and progression. Some of the main symptoms include:
(Healthdirect 2021; Parkinson’s News Today 2021; Better Health Channel 2020; Michael J. Fox Foundation 2019)
While tremors are often associated with Parkinson’s, they only occur in 70% of cases (Parkinson’s Disease 2020c).
At present, provisional diagnosis of Parkinson’s is based on a positive response to levodopa and the following four cardinal symptoms:
(Parkinson’s Australia 2019)
A referral to a neurologist or geriatrician is recommended for specialised diagnosis (Parkinson’s Australia 2019).
(Parkinson’s Australia 2019)
Reactions ranging from anger to disbelief are to be expected from patients when they receive a diagnosis of Parkinson’s Disease. Support and education are integral to overcoming the shock of a Parkinson’s diagnosis. For some, the emotional impact of the diagnosis may outweigh the physical limitations in the early stages (Parkinson’s Australia 2019).
There is not yet a cure for Parkinson’s disease. However, symptoms can be managed effectively by observing the following:
(Healthdirect 2021; Parkinson’s Australia 2020c)
There have been multiple exciting developments in surgical responses to Parkinson’s in recent years.
Deep brain stimulation (DBS) is the process of using mild electric impulses to stimulate a chosen area of the basal ganglia in the mid-area of the brain (Parkinson’s Australia 2018).
DBS is the primary surgery used for Parkinson’s treatment. Note this is not a cure, but a method of managing symptoms - particularly movement symptoms such as slowness, stiffness and tremors (Fight Parkinson’s 2021).
As a result of DBS, a patient may be able to reduce their medication. To be a candidate for DBS, a person will need to meet certain criteria. As with all surgery, there are significant risks involved (Parkinson’s Australia 2018).
Lesioning is the process of making selective damage to certain cells in a specific area of a person’s brain (Fight Parkinson’s 2021).
Lesioning surgery can be an effective treatment, but it isn’t recommended for most people because it may cause irreversible side effects (Fight Parkinson’s 2021).
Rehabilitation programs from an interprofessional team including doctors, physiotherapists, occupational therapists, speech therapists, palliative care services and specialist nursing care can be very beneficial for people with Parkinson’s.
Physiotherapy may help to decrease disability, and regular exercise has many benefits for the individual, including increased muscle strength and flexibility, reduced muscle cramping, improved posture, improved coordination and balance and improved control over gross body movements. A rehabilitation program can ensure a patient with Parkinson’s receives holistic care and treatment whilst in a supportive environment (Greenwood et al. 2013).

When a patient with Parkinson’s is in hospital, it is the nurse who has the most direct care with them. This means they are able to observe the patient's level of function throughout the day and assist with implementing strategies to improve it.
Nurses need to display patience and understanding when caring for patients with Parkinson’s, as patients may need a long time to complete activities of daily living, and their level of function may fluctuate from one day to the next.
As with any degenerative neurological disorder, the effects of Parkinson's are widespread. Care needs to not only address the physical effects Parkinson's has on the body, but also the patient's emotional, psychological and social needs. Therefore, support for these individuals and their carers is essential, and as nurses, we can help provide this support (Greenwood et al. 2013).
Parkinson’s is not considered fatal, however, the progression of the symptoms can considerably reduce a person’s overall quality of life (Parkinson’s News Today 2021).
There are multiple effective treatments available to manage and offer considerable relief for the symptoms of Parkinson’s disease. In some cases, surgery is an appropriate treatment. Interprofessional treatment by physiotherapists, neurologists, dietitians and counsellors may be recommended (Healthdirect 2021).
Question 1 of 3
What is the global number of people affected by Parkinson’s disease is?