Central Line-Associated Bloodstream Infections (CLABSI)
Published: 27 April 2023
Published: 27 April 2023
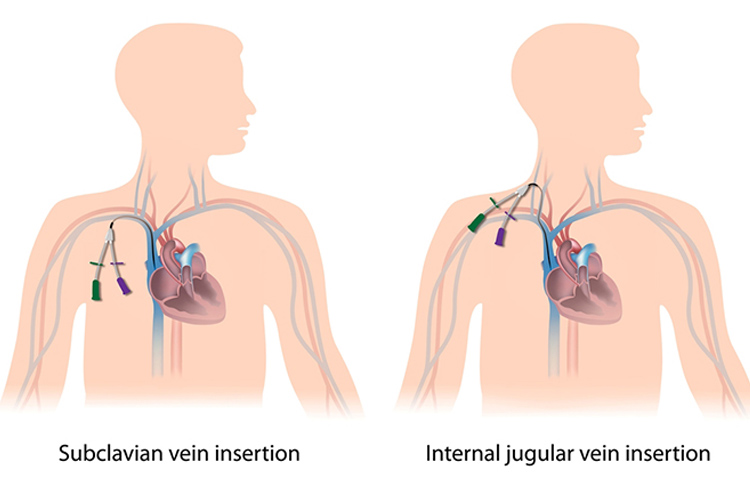
A central line, like the name implies, is a catheter that gains direct entry into the bloodstream with the tip of the line sitting either within the superior vena cava or inferior vena cava, or within one of the great vessels of the neck.
As a result of its central location, this type of catheter can occasionally allow pathogens to gain direct entry into the bloodstream. If this occurs, because of the location of the catheter, patients become unwell very quickly.
This is why prompt assessment, recognition and treatment of central line-associated bloodstream infections (CLABSI) are essential to help ensure favourable patient outcomes are achieved.
The Australian Commission on Safety and Quality in Health Care (ACSQHC) (2019) states that one of the following criteria needs to be met in order for a patient to be diagnosed with a CLABSI:
| Criterion 1 | |
|---|---|
|
|
|
OR
| Criterion 2 | |
|---|---|
|
|
|
|
|
(ACSQHC 2019)
As you can imagine, the cost of CLABSI in both healthcare dollars and patient morbidity is high. Each CLABSI episode increases the length of the patient’s hospitalisation as well as substantially increasing the cost of their healthcare (Haddadin et al. 2022). Therefore, it’s important to be aware of the causes of CLABSI and how we can prevent them from occurring (ACSQHC 2019).
There are many different ways in which contamination of the central line can occur and cause infection. These include:
(Haddadin et al. 2022)
Patient-related risk factors for developing a CLABSI include:
(Haddadin et al. 2022; Chopra et al. 2013; WHO 2016)
Other risk factors include:
(Haddadin et al. 2022; Chopra et al. 2013; WHO 2016)
Central line related infections can be either localised or systemic.
Symptoms of localised infection may include:
(Haddadin et al. 2022)
If a localised infection is suspected, a swab can be taken from the central line exit site if exudate is present.
Symptoms of systemic infection may include:
(Haddadin et al. 2022; MedlinePlus 2022)
If a CLABSI is suspected, a full septic screen of the patient should occur. This will often involve the following investigations:
(Haddadin et al. 2022; ACSQHC 2019)
Treatment of a CLABSI needs to commence promptly. Specific management will depend on the causitive pathogen, patient factors and the patient’s overall clinical status. Blood cultures should be taken to identify the causative organism, and empiric treatment should be commenced while awaiting these results. Generally, antibiotics that cover both gram-positive and gram-negative bacteria will need to be administrred. Once blood culture results are available, more specific therapy can be commenced (Haddadin et al. 2020).
The CVAD may also be removed. If it is to be removed, then the catheter tip may be sent to pathology for cultures. Prior to removal, blood cultures may also be taken via the CVAD (Haddadin et al. 2020).

One of the most important factors of management of a central line is the nursing management of the device and the patient. This not only includes assessing the patient for risk factors for potentially developing an infection, but also means ensuring preventative measures are in place and management of the central line occurs using aseptic non touch technique.
The use of maintenance checklists as well as insertion bundles can also be used to standardise central line care and have been found to reduce the incidence of CLABSI from occurring (ANZICS 2019).
The nurse must manage the central line according to their local hospital policy and procedures, however, this management may include the following:
(CDC 2015; Chopra et al. 2013; Haddadin et al. 2022)
Healthcare professionals should also educate patients in the management of their central line and how they can help protect themselves against a possible CLABSI. Encourage patients to:
(CDC 2011)
The healthcare professional must also monitor for any signs or symptoms of a CLABSI, as well as other complications such as air embolism, catheter damage, catheter migration and occlusion.
In the management of central lines and prevention of CLABSI, the role of the healthcare professional is essential.
Question 1 of 1
In order to be diagnosed with a CLABSI, a patient must: