Skin Tear Prevention and Management
Published: 15 May 2023

Published: 15 May 2023

Despite seeming like minor injuries, skin tears can be complex wounds with the potential to significantly affect a patient’s health and cause chronic discomfort (LeBlanc 2019).
Skin tears are often misdiagnosed and underreported, and in many cases are preventable (Wounds International 2018).
The International Skin Tear Advisory Panel defines a skin tear as:
‘A traumatic wound caused by mechanical forces, including removal of adhesives. Severity may vary by depth (not extending through the subcutaneous layer).’
(LeBlanc et al. as cited in ISTAP 2022)
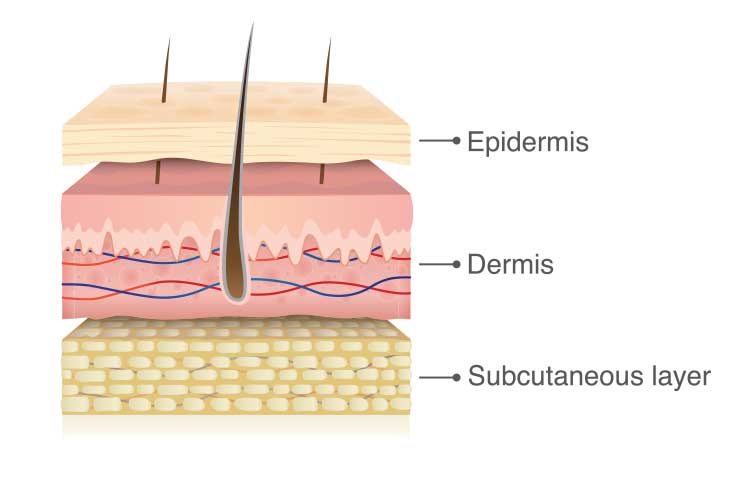
Skin tears are acute, traumatic injuries caused by shearing, friction or blunt force wherein the layers of skin are separated. This may be a separation of the epidermis from the dermis (partial thickness) or separation of both the epidermis and dermis from underlying structures (full thickness) (Wounds International 2018).
Any part of the body can be affected by skin tears, but 70 to 80% of tears occur on the arms and hands (Wounds International 2018).
Skin tears most commonly affect those with fragile skin, particularly older adults (Wounds International 2018).
The physiology of skin undergoes several changes with age, causing it to become more fragile and vulnerable to trauma:
(Wounds International 2018)
These changes, in tandem with reduced skin regeneration abilities and a weakened protective immune system, mean that an older adult’s skin integrity can be damaged by even a small amount of force (Wounds International 2018).
Factors that increase the risk of developing skin tears include:
(LeBlanc 2019)

Identifying at-risk patients through a holistic skin assessment on admission is crucial in the prevention of skin tears (Wounds International 2018).
The healthcare worker should assess:
(Wounds International 2020)
A risk reduction program checklist should be implemented for patients deemed at-risk. See: Best Practice Recommendations for Holistic Strategies to Promote and Maintain Skin Integrity (p. 13).
When caring for patients at risk of suffering skin tears, healthcare workers should take the following measures:
(Wounds International 2018, 2020)
Correct and prompt identification of skin tears is essential in the effective management of the wound. A thorough examination of the skin tear as well as a holistic patient assessment (see above) should be performed upon presentation (Wounds International 2018).
The following should be documented as part of the skin tear assessment:
(Wounds International 2018)
Australia uses the Skin Tear Audit Research (STAR) classification system to distinguish between different types of skin tear. The STAR system comprises five categories:
| Category | Edges | Colour of skin or flap |
| 1A | Edges can be realigned to their normal anatomical position (without excessive stretching). | Not pale, dusky or darkened. |
| 1B | Edges can be realigned to their normal anatomical position (without excessive stretching). | Pale, dusky or darkened. |
| 2A | Edges can not be realigned to their normal anatomical position (without excessive stretching). | Not pale, dusky or darkened. |
| 2B | Edges can not be realigned to their normal anatomical position (without excessive stretching). | Pale, dusky or darkened. |
| 3 | The skin flap is completely absent. |
(Adapted from VIC DoH 2015)
While the STAR system is common practice in Australia in Japan, the International Skin Tear Advisory Panel (ISTAP)’s system is used in other countries (Wounds International 2018).
Prompt and appropriate treatment of skin tears improves patient outcomes. The goals of treatment are primarily to:
(Wounds International 2018)
The process of treating skin tears is as follows:
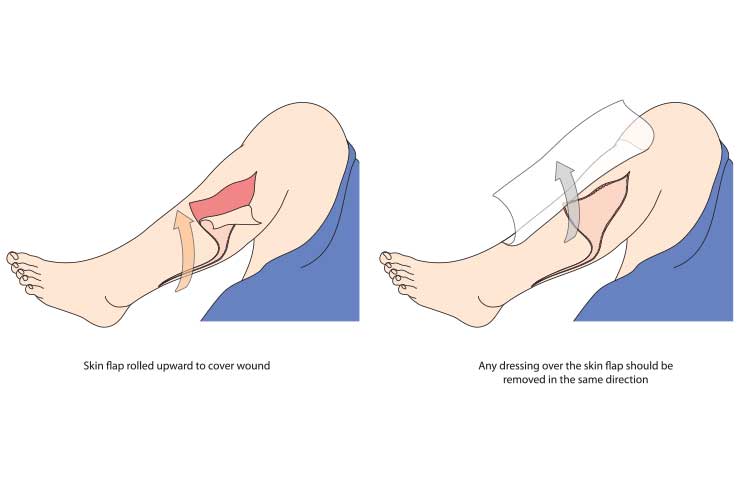
(Wounds International 2018; VIC DoH 2022)
If skin tears are not properly treated, complications such as pain, delayed healing, infection, cellulitis or sepsis may arise (LeBlanc 2019).
If a skin tear does not heal within four weeks, it is considered chronic (Wounds International 2018).
Despite being common among older adults, skin tears are preventable and treatable. However, thorough patient assessment and the ability to recognise and categorise skin tears are essential.
Note: This article is intended as a refresher and should not replace best-practice care. Always refer to your facility's policy on preventing and managing skin tears.
Question 1 of 3
True or false: Most skin tears occur on the arms and hands.